The past few decades, many scholars have emphasized that routines are crucial for how organizations accomplish their tasks (Cyert & March, 1963; Nelson & Winter, 1982). Routines are “recognizable, repetitive patterns of interdependent action carried out by multiple actors” that structure work and are a basic necessity to carry out complex work in organizations (Feldman, Pentland, D’Adderio, & Lazaric, 2016, p. 505; Feldman & Pentland, 2003; Novak et al., 2012). Routines were mostly associated with stability and inertia (Cyert & March, 1963; Nelson & Winter, 1982) but a more recent perspective in the literature explicitly focuses on routines as a source for coping with complexity and change (e.g., Becker et al., 2005, Feldman & Pentland, 2003; Feldman et al., 2016; Parmigiani & Howard-Grenville, 2011).
Building on this, studies paid explicit attention to how organizational routines are changed triggered by exogenous events (Nigam, Huising, & Golden, 2016). Fundamental transitions in the context of work, such as new governmental regulations, knowledge and technologies, client demands and budgetary restraint (for an overview see Noordegraaf, 2015; 2016) explicitly affect work in professionalservice domains and urge professionals to adapt their ways of working.
More specifically, the complex interplay of service pressures has made professional service delivery more multifaceted, and this calls for multi-professional action (Noordegraaf, 2011; 2016). Multi-problem cases in youth care, law, social work, and healthcare require cooperation between various professionals. They might come from different (sub)disciplines. Professionals need to find ways to organize collaboration and create new routines that are connective (Noordegraaf, 2016; Noordegraaf, Schneider, van Rensen, & Boselie, 2016; Noordegraaf, van der Steen, & van Twist 2014). Put differently, the “recognizable, repetitive patterns of interdependent action carried out by multiple actors” need to be reconfigured to routinize collaboration.
Professional fields increasingly implement specific artefacts—formal, “physical” rules such as checklists, standards, forms, and guidelines (D’Adderio, 2008; Pentland & Feldman 2008)—to deal with new demands and organize connective professionalism (Noordegraaf, van der Steen, & van Twist, 2014). Examples are standards for feedback and peer-to-peer learning among judges, or safety checklists for surgical teams (e.g., Haynes et al., 2009). However, it proves difficult to incorporate new artefacts in daily work processes. They do not necessarily result in collaborative action (Pentland & Feldman, 2008; see, for example, Creedon, 2005; van Klei et al., 2012).
In this paper, we analyse professional work practices in which such artefacts have been introduced. We do not so much analyse how these artefacts have been introduced, and how they are used by (individual) professionals, but how they work in-between professionals—how multiple professionals work with (or against?) them, and whether and how they connect the work of different professionals. We focus on checklists that are used by medical professionals in surgical care teams. By combining insights from routine theory and insights coming from the sociology of professions, we study whether and how medical professionals cope with checklists, and whether and how these checklists—as connective artefacts—are actually securing collaboration. We apply ethnographic methods: we observed surgical care teams in action, in a Dutch hospital, and analysed the daily usage of checklists. By studying professional action, we describe how checklists are used and which conditions affect collaboration. We do so with an eye on lessons for health care but also for other professional services.
Theoretical perspective
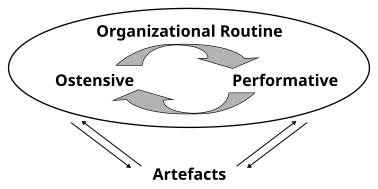
The idea of actors performing, and consequently adapting routines, demarcates a breakthrough in thinking about routines as a source of flexibility and change. Feldman and Pentland (2003) conceptualized internal routine dynamics by discerning two dimensions that make up routines: ostensive and performative. The ostensive dimension is the abstract, generalized idea of the routine. It relates to structure. The performative dimension consists of “actual performances by specific people, at specific times, in specific places.” It relates to agency. In other words, the ostensive dimension is the idea; the performative dimension is the enactment (Feldman & Pentland, 2003; 2005, p. 795). Besides, the authors distinguish artefacts as factors that enable or constrain routine dimensions. Artefacts take on visible and tangible forms, such as written rules. Feldman and Pentland (2003; 2005) recognized a recursive cycle of performative and ostensive aspects affected by artefacts. This dynamic produces both stability and change.
“Designing” routines—a complex matter
Since routines entailmultipleactors inmultipleinteractions, Feldman and Rafaeli (2002) suggest that routines make connections between individuals. People connect through the performance of routines and then create shared understandings on two levels: on a micro level (1) shared understandings about a particularinstance of the routine being performed in its specific context, and on a macro level (2) these connections lead to shared understandings about the broader goals of the organization, backed with ideas about what is appropriate (Feldman & Rafaeli, 2002).
These shared understandings are vital for organizations. Although organizations aim to “plan” and “implement” routines—that is, make a new artefact routine behaviour—there is an essential element of interpretation in routinizing these artefacts. “Seemingly routine behaviour in organizations frequently involves human beings making interpretations regarding appropriate actions to be taken in a particular context” (Feldman & Rafaeli, 2002, p. 321).
Managers often introduce a bunch of artefacts to create a new routine. Sometimes they get the result they want, “but often they do not” (Pentland & Feldman, 2008, p. 235). The artefact thus reflects the managerial idea of the new routine, but the concrete expression of the artefact might differ from the written rule on paper. It is essential to recognize that the routine in practicethat emerges might differ from the routine in theory(see also D’Adderio, 2008).This resembles Brunsson and Jacobsson (2000, pp. 127128) distinction between “standardising practice” and “practising standards.”
Different perspectives on implementation
The implementation of new artefacts such as standards, aimed at creating new routines, has attracted considerable attention from various scholars from different disciplines. Different insights lead to different explanations of differences between routines “in theory” and routines “in practice.”
Complying with standards
Although in routine theory the difference between the two routine dimensions, artefacts, and their interaction is widely recognized, it is attractive to focus on implementing standards. The implementation of new artefacts might be considered a rather “technical” matter. New artefacts such as checklists are seen as simple and cheap solutions to transform professional practice (see, for example, Treadwell, Lucas, & Tsou, 2014, claiming that surgical safety checklists “represent a relatively simple and promising strategy”).
Studies that adopt this instrumental approach often apply a certain kind of measure to scorethe extent to which employees complywith a new standard. These studies mostly rely on professionals’ self-registration data, reporting compliance rates even up to 99% or 100% (see, for example, Fourcade, Blache, Grenier, Bourgain, & Minvielle, 2011; Urbach, Govindarajan, Saskin, Wilton, & Baxter, 2014). It is increasingly acknowledged, however, that checklist compliance in a direct observation study is “a different reality”(Saturno et al., 2014, p. 289). Observational studies report compliance rates that hover around 30% (complete checklist compliance) to 55% (partial checklist compliance) (e.g., van Klei et al., 2012; Rydenfält et al., 2013). Nevertheless, even the few observational studies in the field merely measure whether there is rule compliant behaviour, without taking notice of the context with all its existing work patterns in which the checklist should be adopted.
Moreover, when there is a focus on complying with standards, connections and shared understandings between participants are presented as an outcome of the artefact. Bliss et al. (2012, p. 766, emphasis added) state that “a surgical checklist is an inexpensive tool that will facilitate effective communication and teamwork.” So by these insights, artefacts are seen as simpleand inexpensive tools that will generate connective actions and improve teamwork.
Resisting standards
We might use different insights, which stress social and cultural contexts in which new artefacts are introduced. The implementation of new artefacts might be seen as a social intervention that interferes with taken for granted ways of working (Evetts, 2011). This, in turn, might lead to acts of resistance. Standards are kept at a distance, manipulated, ritualized and/or counteracted.
It is important to note that standardization has always been a crucial aspect of professional work. To reduce complexity, various standards focusing on diverging facets of professional work acted as a form of occupational self-control (Freidson, 1974). To claim a jurisdiction, professionals set educational standards, ethical codes, and codes of conduct. Until recently, these standards thus mainly regulated professional work as case treatment (Noordegraaf, 2016). They did not really interfere with how professionals work together and how they jointly (re)configure professional work, set against new (performance) expectations and demands.
Formal standards, however, are quickly seen as the ultimate bureaucratic instrument, prescribing what to do when and in what ways (Berg, Horstman, Plass, & van Heusden, 2000). This is considered an assault on professional powers, for at least two reasons. First, the standardization of medical work interferes with professional judgment. Professional autonomy enables workers to assess and evaluate cases and conditions and to make judgements regarding advice, performance, and treatment (Evetts, 2002). Standards that prescribe how we should (re)configure professional work interferes with longstanding professional arrangements and is seen/felt as “intrusion” (Evetts 2011, Levay & Waks, 2009; see also Kirkpatrick & Noordegraaf, 2015). Second, standardization of professional work creates opportunities for external parties to exert control over professional work. Increasingly, standards are used by external parties as tools to hold them to account (e.g., Timmermans, 2005). Studies have therefore emphasized the lacking willingness of professionals to implement new standards that cause conflicts with professional values (Freidson, 1994).
What is more, new standards increasingly cross the borders of professional groups. Although there is a shift towards more multidisciplinary service delivery which calls for stronger connections both within and between disciplines, the socializationprocess through which professionals internalize “ways of working” and construct a professional identity takes place within professional segments (Bucher & Strauss, 1960).
The sociology of professions has emphasized how professions not only powerfully shape their members’ perceptions of themselves, but also of others outside their profession, and the “appropriate” patterns of behaviour in relation to others (e.g., Burford, 2012; Freidson, 1994). This creates an emphasis on the difficultiesin generating mutual understandings. It is argued that the different subcultures with their internalized norms, values, and diverging jargon, make the creation of mutual understandings crossing professional boundaries problematic (Abbott, 1988; Lingard et al., 2004). Consequently, a recent and growing body of literature has focused on what professionals do to maintainprofessional powers (e.g., Lozeau, Langley, & Denis, 2002; Waring, 2007). This explains acts of resistance.
Recent empirical findings move beyond notions of mere resistance but report how professionals adapt or capture reforms to strengthen their own position (Levay & Waks, 2009; Waring & Currie, 2009). These more nuanced analyses, however, predominantly depart from an individual standpoint—how individual doctors cope with reforms.
Relational perspective
Although these insights are relevant for understanding how artefacts are used, or not, something is missing in these analyses—they are too instrumental, too political, or too individual.
We, therefore, take routines as our analytical perspective, allowing us to study how professionals work with certain standards together. This is where (contemporary) routine theory can strengthen the sociology of professions, as (a) the ideas about a new routine (ostensive aspects) become very important, (b) the dynamic interrelation between abstract ideas and concrete actions becomes the point of departure, and (c) the relations between professionals become the analytical focus. Feldman and Pentland’s model (2005, Figure 1) conceptualizes routines as dynamic, iterative processes in which “performances” in-between professionals might also influence abstract ideas about the routine.
Beneath, we use the notion of a recursive cycle with ostensive/performative dynamics to understand whether and how medical checklists—as artefacts—affect collaboration between medical professionals, and whether and how more connective professionalism can be witnessed. First, we explain how we collected and analysed data.
Research design and methods
We have relied upon observations of surgical care teams and how they use medical checklists. We analysed the (potential) complexities and contradictions in real-life situations, unfolding in practice, allowing the researcher to capture ambiguities of professional situations and offer a rich explanatory narrative of the mechanisms at work (Flyvbjerg, 2006).
Surgical Safety Checklist
The World Health Organization (WHO) launched its “Safe Surgery Saves Lives” campaign in January 2007. The main goal of the campaign was to improve the safety of surgical care around the world, by decreasing unwanted variety in surgical care and improve teamwork within the OR (Haynes et al., 2009). One of the final outcomes of this program was the Surgical Safety Checklist.
The checklist was designed after extensive consultation of a team of surgeons and anaesthetists (WHO, 2009). Based on the WHO format, the hospital under study introduced the following series of checks that have to be performed at three strategic points in the process: (1) a team briefing at 8.00 a.m. in which each operative patient is briefly discussed by the complete operating team (surgeons, anaesthesiologists, and assistants) to review critical items such as patient identity, planned procedure, required materials, and known allergies, (2) a time-out just before incision, when again these items have to be checked, and (3) a sign-outwhere crucial items have to be checked before the patient leaves the OR, for example, if all gazes and needles have been removed, and where team members have to agree upon and register proceeding therapies.
Information about the new checklist was disseminated among the staff during several meetings and by e-mail. In addition, the checklist was made available in poster format in every operating theatre as well as electronically in the software system.
Research setting
This paper presents fieldwork conducted in 2015 and 2016. Over the course of fourteen months, the researcher undertook multiple field visits to the surgery department of a teaching hospital in the Netherlands. Approval for the study was obtained via the hospital board and the heads of the various departments. In order to formally gain access to the hospital under study, the researcher was appointed as “a research assistant” and to ensure the privacy of patients, had to sign a confidentiality agreement (CA). Before commencing the fieldwork, the researcher visited each key informant to inform and answer questions. The conversations all lasted between 40 and 60 minutes.
Data collection
A focused ethnographic methodology was adopted because it enables a close observation of the day-to-day activities of medical professionals. “Focused” in this approach refers to its problem orientation, as in case of FE the topics of inquiry are pre-selected (see, for example, Higginbottom, Pillay, & Boadu, 2013). Although the focus of this study thus was clearly demarcated in advance—Surgical Safety Checklist, artefacts, ideas, action, connections—this qualitative method using an inductive paradigm to gain in-depth understandings differs from deductive (observational) studies that might fail to capture an in-depth perspective. We especially related the checklists to day-to-day complexities and the real-life mechanisms that affect how and why checklists are used (or not).
Data collection involved observation of everyday work using a shadowing technique, in situ informal interviews as conversations (Mishler, 1996) arising during the course of observation, the collection of documents and attendance at meetings. As such, the data presented in this article are not gathered from formal interviews and stem mostly from participant observation and informal conversations.
There was a specific pre-selected focus on the checklist, but as this study’s aim was to find out as much as possible about the routines and interaction of workflows professionals are engaged in, we decided to observe full working days. To get access to the normally “closed world” of the surgical department, a shadowing technique made a valuable contribution (see, for example, McDonald, 2005). We started with purposive sampling, where we, together with a “gatekeeper,” identified key actors. Subsequently, snowballing led to the selection of other relevant actors that were willing to participate. Although we only shadowed the contact persons, during our days at the surgery department, we also interviewed many additional respondents, like full professors, division leaders, medical doctors in training, OR assistants, and nurse anaesthetists.
Observations were carried out over a period of fourteen months. Observation days lasted for approximately 10 hours, providing a total of about 140 hours of observation, carried out across the different physical areas of the department, including operating theatres, anaesthetic rooms, holding, recovery, training and meeting rooms, corridors, coffee room and changing room. Table 1 provides an anonymized overview of the data collection.
This method to collect data generated possibilities to gather information about the three different routine dimensions. Firstly, observations provided information about the actual performances by specific people, at specific times, in specific places (performative). What do they do, especially together, when they treat cases? These observations also gave insight in the specific physical setting, and the presence of written rules and procedures (artefacts), including the checklists as a physical or digital artefact. Lastly, conversations provided information about the ideas and (shared) understandings of the participants (ostensive). The conversations also helped to reflect on the gathered data with participants, and link the three routines dimensions in order to get a grip on how they are interrelated.
Table 1.
Overview of the data collection.
|
Activity |
Division/contact person |
|---|---|
|
Conversation (acquaintance/exploratory) |
Anaesthesiologist I (*Gate keeper) |
|
Observations (shadowing) |
Anaesthesiologist I |
|
Observations (shadowing) |
Anaesthesiologist I |
|
Observations (shadowing) |
Anaesthesiologist I |
|
Conversation (reflective/progress) |
Anaesthesiologist I |
|
Open interview (implementation SCC) |
Anaesthesiologist II |
|
Observations (shadowing) |
Anaesthesiologist III |
|
Observations (shadowing) |
Anaesthesiologist III |
|
Observations (shadowing) |
Anaesthesiologist IV |
|
Conversation/analysing video footage SCC |
Senior researcher, Quality & Safety I |
|
Conversation (formalising UMCU appointment) |
Anaesthesiologist V |
|
Conversation (reflective/progress) |
Anaesthesiologist I |
|
Conversation (progress/appointment UMCU) |
Senior researcher, Quality& Safety I |
|
Conversation (acquaintance/exploratory) |
Gynaecologist I |
|
Conversation (acquaintance/exploratory) |
Vascular surgeon I |
|
Participation/observation (compulsory) activity for new employees (Module Quality & Safety) |
Not applicable |
|
Conversation (acquaintance/exploratory) |
Orthopaedic surgeon I |
|
Conversation (acquaintance/exploratory) |
Gynaecologist II |
|
Conversation (acquaintance/exploratory) |
Trauma surgeon I |
|
Observations (shadowing) |
Orthopaedic surgeon I |
|
Conversation (acquaintance/exploratory) |
Thoracic surgeon I |
|
Observations (shadowing) |
Gynaecologist I |
|
Observations (shadowing) |
Thoracic surgeon I |
|
Observations (shadowing) |
Gynaecologist II |
|
Observations (shadowing) |
Vascular surgeon I |
|
Observations (shadowing) |
Trauma surgeon I |
|
Observations (shadowing) |
Orthopaedic surgeon I (outpatient clinic) |
Data analysis
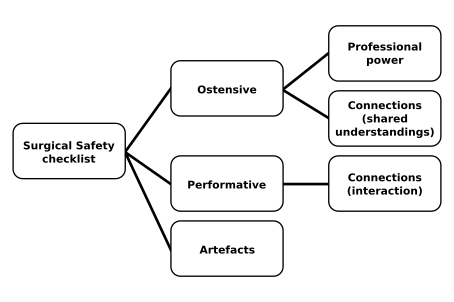
The ethnographic field notes were jotted down in a notebook and meticulously worked out in digital format after every episode of data collection. Both observation and conversation data were imported into Nvivo10 software for the purpose of thematic content analysis. We started off with an initial coding scheme (Figure 2) listing the two routine dimensions and artefacts. These codes are presented as three separate codes for analytical purposes, though we acknowledge that in practice they are constantly interacting and thus might be more “blurred.” Although we included artefacts in the analytic scheme, most emphasis in this paper was on ostensive/performative dynamics. For both these codes, we developed a subcode that reflects the connections; on the ostensive dimension, they refer to shared understandings (ideas), on the performative dimension they refer to actual interactions. The unit of observation was “action,” whilst the unit of analysis was patternsof action.
Informed by the sociology of professions literature, we also included a sub-code “professional power” at the ostensive dimension, to incorporate professionals’ ideas regarding the new standard. During the empirical process, we identified other relevant themes and inductively added thematic codes. “Team stability” for example, emerged as an important factor explaining differences in routines that were created. Further, practical circumstances strongly influenced the ostensive and performative dimensions and were added as a code.
The empirical findings will be presented beneath, revealing conditions under which connective routines can emerge. The results are structured along the themes that emerged and are specifically discussed in terms of ostensive/performative dynamics. The data was used to explore the processes of connective routines as social, situated and ongoing activities. Our aim was not to trace the implementation process in a longitudinal study but to get an in-depth understanding of how surgical teams jointly work with (or against) the checklist.
Results
The hospital where the fieldwork of this study was conducted had introduced the Surgical Safety Checklist in 2009. At the time, the implementation of the checklist was considered a more or less “linear process” that would, if well prepared, lead to the adoption of the new standard. To prepare the staff for its introduction, information about the checklist was shared during staff meetings and through e-mails and the electronic system. Posters were put up in the operating theatre as a reminder.
Three years after its introduction, the hospital performed a retrospective cohort study to measure if the implementation of the checklist indeed had led to a reduction of in-hospital mortality. Although the study found a correlation between the two, a striking result of the study was that compliance did not exceed “average.” The numbers of this self-evaluating study indicated that the checklist was used in practice, but also that there are “barriers” for fully incorporating them. Conversations with various key actors revealed that the hospital was having a hard time in finding clues for “lacking implementation.” Possible explanations remained rather general; “It is something cultural I guess” or “The staff wasn’t well-prepared enough.” By looking at routines, we were open to a more social and situational explanation of the use of artefacts.
Checklist use by general surgery teams
An explicit purpose of the checklist was to strengthen connections among team members. With more than twenty operating theatres, this large teaching hospital not only has a significant labour force but also a high staff turnover, since multiple employees come and go for educational purposes. As a consequence, the “teams” vary, and people operating together who have never met before is quite ordinary. In order to familiarize team members with one another, the SSC not only includes checks concerning patient identity and intervention but explicitly stipulates that team members introduce themselves before a case by writing their name and function on the whiteboard.
Partial use of the checklist
Halfway the period of episodic observations, several “time outs” had passed by during the days at the various theatres in the general surgery department, and in all these instances, the time out was performed in “some kind of way.” Mostly, the first items were systematically checked (identity patient, intervention, allergies), while other aspects were often more “loosely” applied and in varying sequence. Every now and then, the names of team members were on the board. However, if any mutations in the team composition occurred, this was not adopted. Moreover, there seemed to be no attention for or vocal confirmation of the names on the board at all. We wondered how this pattern of “selective” performance emerged; the first items were systematically and consequently checked, whereas the items striving for stronger connections were—if at all—more “loosely” applied.
Varying ostensive aspects: The short-term versus the long-term
During a coffee break, a conversation about such selective performance started, and ostensive ideas about the checklist surfaced. Professionals often do attach importance to the time out procedure, yet some items are considered more important than others. Writing down the names of all the team members, for example, does not add to the safety and quality of the specific surgery performed is the dominant conviction. In other words, there mostly is a focus on the short-term—performing a high-quality surgery—and with regard to that, writing down the names of the team members is not immediately considered to attach value to the quality performance of the operation.
However, a conversation with an anesthesiologist brings forward a different version of the ostensive dimension that emphasizes long-term effects. Writing down the names of team members on the board will strengthen connections between routine participants on the long-term:
We are such a large hospital that it is impossible to know everybody by name. In that respect, just reading the others’ names on the board makes it easier. If I don’t have to ask, “hey you, can you give me that ampule” it becomes easier to communicate, and I am more inclined to ask more personal stuff like “how was your weekend,” you see?
Writing down the names serves a broader purpose—it does not only mean that team members basically know each other’s names, but it is also an attempt to form more in-depth connections that could ultimately lead to more shared understandings.
These views that reflect different understandings of the ostensive dimension of the time out—rooted in focus either on the short- or long term—explain differences in the performative dimension.
Performing the checklist, but not connective
The performance of the checklist requires interaction among the various team members. Every individual participating in the team must be able to communicate about the various items and “pause” the process in case the requirements of items have not yet been met. The findings show that for creating connective patterns of action, the hierarchical position matters.
The following observation note reflects the performance of a time out procedure in the general surgery department.
Time out
Surgeon: People, can we please first do the time out? Where is everybody? I have a full schedule today!
Anaesthesia assistant: [Walks towards the neighbouring room where the operation is being prepared to get the other team members.]
Surgeon: Okay, is everybody there? Thank you. [Does the time out and then leaves the operating room.]
The anaesthesiologist starts to administer drugs for general anaesthesia. When the patient is asleep, about ten minutes pass by.
Anaesthesiologist: [annoyed] Who is waiting for who now?! She could have started surgery ten minutes ago. She was pressing to do the time out and look what happens now; we don’t even know where she is!
In this performance of the time out, the first items of the checklist were consistently checked in interaction with the patient. However, the surgeon performing the checklist finishes the procedure by checking for allergies and herewith neglects, for example, hygiene items and team composition. The fact that one of the assistants “mumbles” these items and writes down the names on the board herself indicates that she is aware of the incomplete performance of the time out. Nonetheless, she does not communicate about these items with the other team members.
Varying ostensive aspects: Equal teams vs hierarchy
The working situation hindered the possibility to immediately ask for further clarification—why did the assistant mumble? A conversation later on, however, focuses on the experienced hierarchical relations. This OR assistant is finalizing her education, and because of her educational program, she has worked at various surgical departments to get acquainted with the diversity of surgical interventions. The observation note reflects the conversation we had about the performance of the time out in various contexts.
OR assistant: The performance of the time out differs widely. In some instances, it is just very quick and superficial, while in other cases, it is a rather extended procedure in which all items on the checklist are also written down.
I: How do these differences occur you think?
OR assistant: I think it has to do with how approachable the doctors are, and whether it’s a ‘real’ team. It has to do with the atmosphere, whether there is a pleasant and open atmosphere. Sometimes, you have the feeling that we are all equal, and then it [the checklist] goes smooth. Especially with the older doctors, you notice that it’s more hierarchical.
This conversation shows how individuals high in the hierarchy play a key role in the emergence of connections. Team members refer to a “pleasant atmosphere” and the existence of “a real team” as requisites for performing the checklist together. The surgeons—who often lead the checklist procedure—are indicated as the actors responsible for the atmosphere in the theatre. If other team members feel free to speak out, they are more inclined to participate in the team discussion and interrupt when necessary. However, if the surgeon explicitly presents him or herself as leader of the team and others do not feel that they are “all equal,” it becomes more difficult to cross these hierarchical borders. In these situations, there is attention for the checklist, for example by the assistant who mumbles and completes the items by herself, but not in a connective matter.
Checklist use by specialized surgical teams
Although most surgeries are performed in “variable” teams and an explicit purpose of the checklist was to create firm connections among team members, there are a few subspecialties where teams work together in more stable compositions. Subspecialties such as thorax surgery and vascular surgery are forms of very specialized work that require more stable teams. Anaesthetists that work in thorax surgery, for example, only work in these specialized areas. Therefore, fixed teams emerge in which surgeons, anaesthetists, nurse anaesthetists, OR assistants, and specialists that operate the cardiopulmonary bypass machine frequently work together. Because of these frequent encounters, these teams have the possibility to create shared understandings about what has to be done and what is appropriate.
Performances: Deciding on the spot
Observations were conducted at both the departments of vascular and thorax surgery to see how these specialized teams work with the SSC. The observation day at the thorax surgery starts at 8.00am in the operating theatre. The team immediately starts with the time out—the second part of the checklist. Since all team members only have responsibility for operations in this OR today, everyone is present in time. The thorax surgeon starts the time out and checks the patient’s identity, allergies, and prosthetic devices, and he performs the procedure entirely from memory.
After the time out, the surgeon leaves the OR to scrub, while the residents, nurse anaesthetists, and OR assistants prepare the patient for the surgery. Interestingly, when the patient is asleep, the team members are making ‘fun’ with each other while doing their jobs, for example, by squirting water from injection needles in each other’s ears. People not only know each other by name, but they also seem to get along quite well and work in a “relaxed” atmosphere.
A couple of minutes later, the surgeon is operating the first patient of the day. While he is working, the next patient is already discussed in an informal way. Statements like “what shall we do”, “you tell me!” and “we’ll get there” pass by. Though the “plan” for the next patient is discussed on the spot—comparable to what a briefing stipulates—this conversation is not systematic and moreover, required equipment is not yet resembled at the start at the day, as the checklist prescribes.
Two hours later, the operation is finished. While the assistants are cleaning up the OR, the surgeon asks: “Did we do the sign-out?” The other team members nod approvingly. “Oh, I missed that. That’s not quite right actually.” He replies. When the next patient on the table, the surgeon takes the lead in the time out again. Just like the case before, he checks the identity, intervention and prosthetic devices out of memory. The performance here deviates from the prescribed items on the checklists; some items are not covered, whilst others (prosthetic devices) are added to tailor the checklist to the needs of this specific context.
Ostensive aspects: What actually “is” the routine?
A few minutes later, when the patient is on the table, and the time out has just been performed, we start a conversation with the resident in thorax surgery to ask him about the briefing. The observation note covers the short conversation.
I: Do you also have a team briefing?
Resident in surgery: This was the briefing
I: No, this was the time out, the last check right before incision of the skin.
Resident in surgery: Oh, no. We don’t have a briefing then.
Some confusion occurred, since the resident was convinced that they do work with the checklist—they indeed “performed” some deliberation regarding the patient. However, it turned out that this team had altered the checklist through recurring performances in such a way, that it deviated from the artefact as such. In this case, strong connections among team members—that thus already exist—seem to encompass a lot of trust among team members in which people are inclined to rely on each other’s performances rather than explicitly checking the items with one another. Table 2 summarizes the findings covering the internal routine dynamics.
Table 2.
Summary of findings of the interrelation of routine dimensions.
|
Performative |
Ostensive |
|---|---|
|
General surgery |
|
|
Selective, partial use of the checklist Checking identity, procedure, allergies Putting team member names on the board Not putting names team members on the board |
Important items for patient safety Will ultimately lead to better teamwork (long-term) Does not add to quality of the surgery performed (short term) |
|
Individual, not connective use of the checklist Individual actors perform items of the checklist but not in collaboration Connective use of the checklist (high ranked professionals playing frontrunner role) |
Senses of hierarchy (not speaking up) Feelings of a “pleasant atmosphere” |
|
Specialized surgery (vascular, thorax) |
|
|
Informal checking, not using checklist Checking safety items, but loose and without artefact Tailoring the checklist to local circumstances (e.g., adding prosthetic devices) |
Not clear what the routine is; “this is how we do things” |
|
Partial checking, but not as a whole team |
Entrusting others |
Practicalities and unexpected events that affect routine dynamics
Although our initial focus was on the internal routine dynamics, the interaction with existing work routines showed great influence on these dynamics.
The surgery department schedules the various operations in which mostly one surgeon is responsible for the surgeries in the operating theatre planned that day, for example, a range of hip fractures or colon carcinomas. The anesthesiologists on the other hand, are responsible for at least two of these operating theatres at the same time, which not only means that they have to monitor two patients at the same time, but also that they have to attend two briefings and time outs “at the same time.” The observation record shows how the organization of the time out in the care process leads to “basic” irritations, simply because people have to wait for one another.
This situation reflects the importance of the embeddedness of the new artefact within existing practices. The organization of the care process makes it difficult to create a new connective routine within this high-paced, demanding environment. The checklist aims to connect the different professional segments and improve their collaboration, the lack of “fit” with the existing workflows, however, not only hinders the creation of a connective routine, but the basic irritations tend to reinforce segmentation and thus stimulate the opposite effect.
Comparable practicalities emerged for example with “two-part surgeries,” where two different surgeons perform different parts of the intervention (for example, a breast mastectomy followed by reconstruction), but have to be present for the briefing and time out together. This routine required professionals to wait for another, interrupt and align their tasks, which proved time-consuming effort. In these instances, the checklist routine interfered with existing workflows, which means that professionals have to improvise and decide “on the spot.” This might imply that the action patterns that emerge deviate from the “rule” as inscribed in the artefact. Nonetheless, these instances of “noncompliance” might very well be best solutions for the situation at hand.
Discussion
In this paper, the case of the Surgical Safety Checklist was used to examine what happens when a checklist that aims to facilitate collaboration is introduced in a professional environment. A micro-level focus on routines allowed us to trace whether and how such a connective artefact is used (or not) in day-to-day professional actions by multiple professionals.
The data show that the routines that emerge often vary from strict prescriptions in the artefact. However, our findings show that these routines are often meaningful patterns that emerge from professionals’ efforts to cope with artefacts in demanding and high-paced environments. Instead of resistance and professionals’ active attempts to restore or maintain the status quo, many connections crossing the borders of professional segments already exist. However, the results also show that communication and collaboration are not “automatic” outcomes of artefacts. On the contrary, they can be better considered as effortful accomplishments (also Feldman et al., 2016). Moreover, communication beyond professional borders is not an outcome but a clear requisite to make checklists work in practice. The findings show that especially individuals in high-ranked positions are key players in establishing connections since they have the position to both help or hinder this process.
In instances where connections appeared weaker, practicalities such as variable workflows and unexpected events made it difficult for professionals to connect. In these instances, the artefact seems to instigate irritations that ultimately reinforce ideas of “us” and “them.” Therefore, although there was no fundamental resistance to the new standard, at first sight, a lack of fit of the envisioned checklist routine with the already existing work routines resulted in more negative attitudes.
We conclude that in professional contexts, it might be more valuable to adopt practices to situational demands, rather than focusing on strict “compliance” with artefacts. We have shown that professionals not so much actively try to preserve old values but pragmatically cope with artefacts in other to find the most convenient way to incorporate a checklist in existing workflows. Connective routines partly already exist. Further development of such routines should result from enduring, repetitive efforts. Organizing connective professionalism is thus a matter of pragmatic coping with artefacts in high-paced circumstances.
These results are in line with a growing body of literature that focuses on the active involvement of professionals in the reconfiguration of professional work. Exogenous pressures not only lead to resistance. Either, professionals actively work with and give shape to reforms (see, for example, Wallenburg, Hopmans, Buljac-Samardzic, den Hoed, & IJzermans, 2016). In the literature on “organized professionalism,” there have been research efforts to overcome the divide between organizational and professional logics (e.g., Kirkpatrick & Noordegraaf, 2015; Noordegraaf, 2011; 2015; Postma, Oldenhof, & Putters, 2015). In this research strand, there is a strong emphasis on the hybridization of logics in professional work.
This analysis adds to this, by explicitly approaching the introduction of new standards as a relational matter. Our analytical perspective focusing on routines is a collective lens and allows for contributions to the literature in different ways. First of all, checklists have been heralded for their simplicity, and health care scholars often refer to the successes of a checklist that led to a reduction of sepsis caused by central lines (see, for example, Pronovost et al., 2006). However, this checklist was developed for individual use to prevent infections. A surgical team checklist fundamentally differs from these individual checklists, since its success is determined by the connections that individuals make in performing the checklist. Nonetheless, explanations for lacking implementation of (team) checklists mostly stick to the individual level. It has been commonly assumed that most of the barriers to “effective implementation,” such as negative attitudes, operate at the level of the individual health care professional (Grimshaw, Eccles, & Tetroe, 2004). An observational study by France, Leming-Lee, Jackson, Feistritzer, and Higgins (2008) on the compliance to a surgical team checklist, for example, focused on the “engagement” of individual professionals. Although we argue that individual attitudes do matter, from our analysis, we claim that they only exist, change—and thus matter, in interaction with others. Our analysis from a routine perspective underlines the collective and therefore social nature of working with standards.
In addition, scholars increasingly differentiate between “individual” and “system barriers” when it comes to standard implementation (see, for example, an overview by Grol & Wensing, 2004). This study shows that it is not so much about different factors at different levels. The analytical perspective enabled us to provide a more social and contextual understanding since routines capture the dynamics in-between the system and the individual level.
Finally, a focus on routines allowed us to trace on a micro-level what action patterns actually emerge. In implementation studies, many different conceptualizations are used to “measure” compliance to standards. Although mostly, the actual use of a checklist (performative dimension) and the registration of the checklist are considered one and the same thing (see, for example, Fourcade et al., 2011; Urbach et al., 2014). Based on our analysis we urge scholars to clearly differentiate between registration data and actual performance. Our findings demonstrate that two separate routines might emerge; one for the performance of the checklist that thus varies widely, and one for the registration of the checklist (ticking off the boxes) that takes place after the actual performance.
Our study is a specific case of a connective artefact used by a particular professional group of professionals (surgical teams). Contextual conditions might have foregrounded particular circumstances. However, we have drawn lessons for healthcare and revealed conditions that could be further explored in other professional domains in future research.
This study gives rise to new research questions. First, it would be worthwhile to shift the focus from routine dynamics to routine interactions. During the empirical work, it showed that the interaction or “fit” with existing work routines affected routinization of the checklist. Practical issues often hindered a smooth routinization process. Therefore, an explicit focus on how new standards interact with longstanding ways of working would be highly relevant. Second, as this paper predominantly focused on the routine dynamics, a closer look at how different representations of the checklist (the artefacts) influence the creation of routines would be highly interesting (see also Feldman et al., 2016). Hospital boards often introduce different artefacts, be it posters, boards or digital versions of the checklist, to stir professional behaviour. Follow-up research might concentrate on how these material representations affect routine dynamics.
Conclusion
We have shown how medical professionals really use medical checklists as artefacts, although we sketch a nuanced picture. First and foremost, medical professionals pragmatically cope with checklists amidst high-paced circumstances. In many ways, they are critical of new standards and they “tick the boxes” whilst working with them, but they also really use standards to improve case treatment. How they do this clearly depends on the nature of cases, time pressures and team composition. Real-life circumstances count and affect the extent to which connective professionalism is established, by forming connective routines. This is partly a matter of ideas, but largely a matter of performances, strongly affected by real-life circumstances.
Connections between professionals, moreover, do not so much result from standards but are a perquisite for using standards. There must be some connective potential when standards for making connections are used. High ranked professionals play important “frontrunner” roles in order to exploit such “connective potential.” When they set the tight tone and stimulate others to collaborate, checklists are used differently, both in terms of ideas and actions. Professionals themselves rather than checklists establish collaboration, but checklists are important devices for actually using such connective potential. Even when they work against connective standards, they might work with each other.
Acknowledgements
We thank all the respondents for their participation in this study. We also thank the anonymous reviewers and ISA RC52 for their constructive comments and suggestions.