Magne Nylenna, Oyvind Bjertnaes, Ingrid Sperre Saunes and Anne Karin Lindahl
What is Good Quality of Health Care?
Abstract: A diversity of definitions of quality exists, that frequently contain aspects of complexity, relativity and subjectivity. This paper provides an overview of key components in the quality debate within health care, including different perspectives and dimensions of the quality of care. Definitions of the quality of health care reflect the characteristics of health services, and are useful for measurements and quality improvement. Over time the patient perspective of quality has gotten increasing weight, and in quality improvement there has been a shift from individual responsibility for doctors and health care personnel to systems thinking. We argue that the quality approach in health care should be more standardized and that health care-specific definitions of quality should be used when the relationship between physician professionalism and quality is investigated.
Keywords: quality; health care; systems thinking; patient perspective; outcome; indicator; measurement; improvement
Studies on physician well-being frequently involve its relation to quality of care. What is the impact of physician job satisfaction on the quality of health care? An understanding of the complex nature of quality is in this context as crucial as an operational definition.
The different perspectives of politicians, physicians, and patients may lead to different judgments of quality. Over time, the patient perspective has got more attention. This, as well as a shift from individual responsibility to systems thinking in quality improvement, has consequences for conceptual models of the relationship between physician professionalism and the quality of care.
We aim at providing an overview of key components in the quality debate within health care. By presenting an analysis and discussion of the development of approaches to and definitions of quality of care we hope to create a better basis for discussions of the relationship between physician professionalism and quality.
The concept of quality in general
Tracing the origins of the quality concept takes us back to France at the beginning of the 13th century, where qualite was used in the meaning of characteristics. A quality (from Latin qualitas) is originally an element or attribute of someone or something, defined as “a characteristic or feature that someone or something has: something that can be noticed as a part of a person or thing” (Quality, 2014).
In everyday language, quality is also used to describe the standard of something or someone, “the degree of excellence” that a thing possesses (Quality, 2014). Normally, this use of quality refers to an overall assessment of several components more or less related to each other, whereas the assessed quality of a service or a product is based on a complex combination of attributes. Some of these attributes might be measurable, such as the regularity of an airline company or the lifetime of a dishwasher. Such an isolated, single characteristic is seldom called quality in itself, but instead is seen as a part of- or indicator of- the total quality of the actual airline or dishwasher.
Quality is usually applied to the standard of several characteristics in combination, frequently including characteristics that are more difficult or even impossible to measure and quantify. For an airline, this could include the passengers’ experience of service, and for a dishwasher how its design is perceived.
Relativity
Most definitions of quality relate the standard of a service or product to something else, thus giving quality a relative value such as poor, good or excellent. This implies a comparison, as the comparator might be more or less well specified and even vary, for example over time.
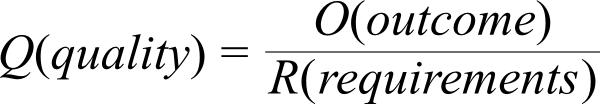
A widely used definition of quality in general is, “the degree to which a set of inherent characteristics fulfills requirements” (ISO, 2005). According to this definition, “inherent,” as opposed to “assigned,” means “existing in something, especially as a permanent characteristic,” while requirement means a “need or expectation that is stated, generally implied or obligatory.”
Whether a product or service meets implicit or explicit requirements is at the core of its quality. In this sense, quality can be seen as the ratio of outcome (result, experience, etc.) to requirements (needs or expectations):
Hence, the quality of an airline or dishwasher depends both on expectation (requirements) and experience (outcome). The outcome is the sum total of measurable (quantitative) and unmeasurable (non-quantitative) results, while the expectation is the anticipated level of these characteristics. This level is usually set through a knowledge of comparable services or products, or other judgments made beforehand.
Based on this relative approach, quality will increase not only by a higher outcome, but also by a lower expectation. For most services and products, the expectations will increase over time, thereby demanding a higher outcome to keep the quality at the same level. Expectations may also vary according to social, cultural, economic and other factors, for example in the airline industry when flights are delayed due to poor weather conditions. Whether passengers’ expectations are adjusted accordingly decides the perceived quality of the airline, and these adjustments are again dependent on information and an acceptance of the consequences that bad weather will have for air traffic. For airline companies and dishwashers, expectations are probably also related to price, since high prices will lead to higher expectations than low prices. If the experiences with a budget airline or a cheap dishwasher are seen as similar to services or products that are more expensive, the quality could be judged as being higher.
Subjectivity
Even based on the more or less same expectations, quality may be judged differently by different individuals. Whether requirements have been met is frequently a matter of disagreement, although this element of subjectivity is different from the described relativity implied in quality judgments. W. Edward Deming (1900-93), who led the quality revolution in Japan and the United States, said that “a product or service possesses quality if it helps somebody and enjoys a good and sustainable market.” The same product or service that might help and satisfy one customer might disappoint another.
Two individuals using the same airline company or buying the same dishwasher may conclude rather differently as to the results or experiences, and therefore also on the quality. This subjectivity can be related to different emphasis on underlying characteristics. A typical example is the diverse judgment of the interior of a dishwasher; is a cutlery basket or a separate cutlery tray preferable? Another example is related to the balance between noise versus the time of a regular washing program of a dishwasher. Some will prioritize time over silence, whereas others will prioritize silence before time.
Quality in health care
Health-care quality and quality indicators are complex topics, with a range of different conceptual approaches, operationalizations and measurement techniques (Arah, Westert, Hurst, & Klazinga, 2006; Legido-Quigley, McKee, Nolte, & Glinos, 2008; Lohr, 1990a; Smith, 2009). Furthermore, the distinction between quality and performance is often unclear, and the level of measurement varies from the concrete practice level to the health-care system level (Adair et al., 2006; McIntyre, Rogers, & Heier, 2001). The fact that patients, clinicians, leaders and other stakeholders might have different perspectives on health-care quality makes it even harder to standardize and harmonize different conceptual models of quality.
Perspectives on health-care quality
It should be noted that the different levels of quality of care are not the same as different perspectives on health-care quality. Various perspectives can be applied within each level of care. These perspectives are strongly related to roles and stakeholders, with the three main perspectives being defined as:
-
Politicians, health-care managers and others with responsibility for groups, communities and national systems;
-
Health-care professionals treating individual patients;
-
Patients and their relatives.
The patients’ perspective differs from that of health-care personnel, and health care personnel’s perspectives differ from that of managers and politicians insofar as: “Where you stand depends on where you sit.” Different roles will normally reflect different values and priorities. Managers will probably emphasize efficiency and a just distribution of resources more than health-care professionals and patients. They might also be more concerned about sustainability regarding research, education and economy than other groups. Physicians, nurses and other professional groups might have other priorities than individual patients, whereas patients are more likely to emphasize the importance of sufficient time in consultations than physicians (Levine et al., 2012).
The patient perspective is important in quality judgments, but the level of importance depends on the chosen definition of health-care quality.
Table 1
A selection of quality definitions (Legido-Quigley et al., 2008).
|
International Organization for Standardization (ISO) (2005) |
The degree to which a set of inherent characteristics fulfills requirements. |
|
Donabedian (1980) |
Quality of care is the kind of care that is expected to maximize an inclusive measure of patient welfare after one has taken into account the balance of expected gains and losses that attend the process of care in all its parts. |
|
Institute of Medicine (IOM) (1990) |
Quality of care is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes, and are consistent with current professional knowledge. |
|
Department of Health (UK) (1997) |
Quality of care is: |
|
Council of Europe (1998) |
Quality of care is the degree to which the treatment dispensed increases the patient’s chances of achieving the desired results, and diminishes the chances of undesirable results with regard to the current state of knowledge. |
|
WHO (2000) |
Quality of care is the level of attainment of health systems’ intrinsic goals for health improvement and responsiveness to legitimate expectations of the population. |
In general, the ISO definition of quality implies a rather relative view of quality by relating it directly to requirements. This opens up the possibility of varying quality perceptions between individuals and between different stakeholders confronted with the same services. The IOM definition relates quality to the goals of the health-care system, as well as to the current level of professional knowledge.
One possible use of the ISO definition is to ask patients what constitutes the most important outcome to them and apply this as the requirement part of the quality definition. A special Euro Barometer population survey on safety and the quality of health care in all European countries conducted in 2009 asked respondents to prioritize different quality criteria (European Commission, 2010). The results of the survey showed that effective treatment and a competent medical staff were considered the most important quality criteria for Europe as a whole. Furthermore, a fair agreement was found on at least the two most important quality criteria across the European countries, but also a lot of between-country variation and some variation between different socio-demographic groups. A Norwegian study showed that it is possible to identify ten core patient experience items across nine patient groups in specialized health care based on patient priorities, including items on safety, effectiveness and responsiveness. This study also showed that certain aspects varied between the groups (Sjetne, Bjertnaes, Olsen, Iversen, & Bukholm, 2011). Consequently, the European and Norwegian studies show that there is no universal definition of quality criteria, even from the patient or population perspective. Other stakeholders with other perspectives, such as managers and professionals, may have other expectations and requirements (Jung, Wensing, Olesen, & Grol, 2002; Levine et al., 2012).
A study comparing physician and patient perceptions of quality found both similarities and differences regarding the quality concept in ambulatory care (Levine et al., 2012), as both groups highly valued clinical skills, rapport and health-related communication, but varied in sub-categories within these topics and on other major topics. The bottom line is that quality is a relative concept according to the ISO definition, and that health-care service quality cannot be judged without linking it to the requirements of patients or other stakeholders.
Deciding on a more specific health-care definition of quality, the patient perspective has an important but more limited role. The patient perspective is included in most conceptual health-care models of quality as a separate quality dimension, and patients are also included in the evaluation of quality. For example, through concepts like patient satisfaction and experiences of care, the IOM approach includes the patient perspective in the term “outcomes,” which also has patient centeredness as one of six dimensions of quality (Institute of Medicine, 2001; Lohr, 1990b). The patient centeredness component is usually measured by systematic surveys of patient-reported experiences, at least in large-scale settings.
The quality triade
In the mid-1960s, Avedis Donabedian (1919 – 2000) raised the question of how the quality of health care can best be assessed (Donabedian, 2005), and introduced what has later become known as the quality triade, namely, structure, process and outcome:
-
Common indicators of structure are economy, buildings, number of hospital beds, population to be served;
-
Process indicators consist of organizational processes (how the organization is working) and clinical processes (interaction with the patient). Examples may be adherence to guidelines, checklists and a communication with patients.
-
Outcome indicators of quality for the patient may be survival, level of functioning, quality of life, patient satisfaction and experiences. Output measures of quality for the organization may be the number of patient-treated and economic measures.
Donabedian wrote that the structure-process-outcome model was particularly relevant for clinical practice, and that it might be less relevant for other settings. There is an ongoing debate on the pros and cons of structure, process and outcome measures, but Donabedian himself pointed to the need for indicators on all aspects. He also claimed that structure, process and outcome indicators together give information that could be used to infer something about quality, but they are not quality per se. Understanding the purpose of the indicator is important when using it to assess quality (WHO, 2006).
The patient experiences are an important component of health-care quality, and as such, are important quality indicators. In accordance with Donabedian’s approach to quality measurement, and based on their experiences with health services, patients can evaluate the structures, processes and outcomes of care. There is a huge amount of literature on the patient evaluation of structures, processes and outcomes, including various concepts such as patient satisfaction, patient-reported experiences, patient-reported outcomes and health systems’ responsiveness. These concepts are partially overlapping but also complement each other, and as a whole constitute a broad approach for the evaluation of health services from the patient perspective. Obviously, other perspectives and stakeholders have a role in the definition and evaluation of health-care quality, but the key importance of the patient perspective has strong support in policy documents and research articles (Arah et al., 2006; Donabedian, 1988; Gerteis, Edgman-Levitan, Daley, & Delbanco, 1993; Legido-Quigley et al., 2008; Smith, 2009).
Dimensions of health care quality
A variety of definitions for health-care quality have been proposed (Arah et al., 2006; Donabedian, 1988; Donabedian & Bashshur, 2003; Institute of Medicine, 2001; Legido-Quigley et al., 2008; Lohr, 1990a; Smith, 2009) (see Table page 4), and most of them relate health-care services to health outcomes. A frequently referenced definition from the Institute of Medicine states that, “quality of care is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (Lohr, 1990a). The IOM definition is health-care-specific and was based on a review of approximately 100 health-care quality definitions (Lohr, 1990b), relating quality to the final goals of the health-care system. Moreover, health outcomes are not specified in detail, opening up the possibility of different perspectives on what are the most important outcomes (Legido-Quigley et al., 2008). The definition includes both the patient and population perspective, thus also including the health promotion part of the health-care system.
However, some common features exist. These can often be traced back to the work of Avedis Donabedian (1919-2000), creator of The Donabedian Model of Care, and who is seen as the founder of the study of quality in health care (Donabedian, 1988, 2005; Donabedian & Bashshur, 2003). Donabedian conceptualized quality as the product of the science and technology of health care and the application of that science and technology, thereby resulting in the following dimensions (Donabedian & Bashshur, 2003):
-
Efficacy, the ability of the science and technology of health care to bring about improvements in health when used under the most favorable circumstances;
-
Effectiveness, the degree to which attainable improvements in health are in fact attained;
-
Efficiency, the ability to lower the cost of care without diminishing attainable improvements in health;
-
Optimality, the balancing of improvements in health against the costs of such improvements;
-
Acceptability, conformity to the wishes, desires and expectations of patients and their families;
-
Legitimacy, conformity to social preferences as expressed in ethical principles, values, norms, mores, laws and regulations;
-
Equity, conformity to a principle that determines what is just and fair in the distribution of health care and its benefits among members of the population.
One early and influential work within this field is attributed to Marc Lalonde, a Canadian Minister of National Health and Welfare, responsible for the report on the health of the Canadian population in 1974 (Lalonde & Department of National Health and Welfare, 1974). The report made two major contributions to the understanding of the field of health care. The first one may seem obvious today: that population health is not only attributable to health care, environmental and social factors are major determinants of health. This insight was an important contribution to the emphasis on preventive and primary health care as stated in the Alma-Ata declaration of the WHO (Irvine, Elliott, Wallace, & Crombie, 2006). The second contribution was identifying eight components of the health-care system contributing to the quality of health care: acceptability, accessibility, appropriateness, competence, continuity, effectiveness, efficiency and safety. Especially interesting are the terms competency, continuity and safety. Ensuring individual competency has been at the focus for the medical professions since the early days of quality assurance, but the emphasis on safety and continuity of care were early recognition of important quality characteristics in an increasingly more complex health care sector.
Nearly 30 years after the Canadian report, The Institute of Medicine (IOM), an independent, non-profit US-based organization, proposed six components that define quality in health care based on a systematic review of the dimensions of quality improvement (Institute of Medicine, 2001). According to this proposal, high-quality health care should be: safe, effective, patient centered, timely, efficient and equitable.
Ensuring competency may be interpreted as a part of efficacy, the ability of science and technology to bring about improvements in health when used under the most favorable circumstances, having competent personnel may be seen as an important prerequisite to achieve improvement. It may be tempting to say that these three classical mapping of quality characteristics as “same, same, but different”. They differ in terms of time of origin, from the beginning of the 70s, to mid- eighties and late nineties, they may differ in perspective, from the Health Minsters policy perspective, to Donabedians’ clinically-oriented perspective, and the later IOM can be interpreted as an attempt to bridge both policy, clinical and patient perspective. There are similarities and there are differences, and the recognition of this lead to yet another systematic review of central health-care performance frameworks. A quality indicator project established by the WHO, OECD and the EU-commission selected effectiveness, safety and patient centeredness as the primary dimensions for comparing quality (Arah et al., 2006). Other, Norwegian approaches, have included these three components, and supplemented them with access to health services, equity, efficiency and an integration of care (Rygh et al., 2010).
Donabedian underscored that the different dimensions of quality depend on the level of assessment, ranging from the care provided by practitioners and other providers to care received at the community level (Donabedian & Bashshur, 2003). For instance, core dimensions for the former are effectiveness, efficiency and the patient-practitioner relationship, while the latter has relatively more focus on legitimacy and equity. Donabedian argued that there is no general answer to the relative priority of different dimensions or what dimensions to include or exclude, but rather that such questions depend on the measurement context. Therefore, according to Donabedian, the measurement of quality depends on a definition of quality, an operationalization of quality dimensions and a selection of dimensions according to the relevant measurement level.
Having decided on a definition of quality, the next step is to operationalize the concept as a basis for measurement and improvement. As for the definition of quality, a range of different approaches exists regarding operationalization. As a result, the dimensions of quality are coming closer to a common approach, but lack a universal standard and should be explicitly chosen and argued for in the context of evaluation. The context could be the health-care system or lower levels of health care, for example a single health-care provider, which affects the priority of and selection of dimensions.
Measuring quality of care
Assessing the quality of care may have different purposes, and can be applied on different levels of the health-care system (Arah et al., 2006). Because the complex concept of quality of care is hard to define and impossible to measure directly, proxy variables and indirect indicators must serve the need.
Quality indicators are limited components of the quality of care, and serve as tools to measure what is not measurable in—and for itself: the overall quality of health care. Quality indicators may either reflect what constitutes quality or reflect the quality of care provided. Aspects that constitute quality are manifold, and incorporate the structures and the processes involved in the delivery of health care. They are the independent variables that cause (whether directly or indirectly) the quality of care. The outcome or output variables are also manifold, and are believed to be reflections of good quality care, and they are caused by care. In the OECD quality indicators project initiated in 2001, they identified three main criteria for selecting the indicators: the importance of what is being measured, the scientific soundness of the measure and the feasibility of obtaining data (Kelly & Hurst, 2006).
The scientific soundness of quality indicators are dependent on both the validity (is the indicator actually an indicator of the particular aspect of quality, and do you measure what you want to measure) and the reliability (can you trust how it has been measured, and does the indicator capture the relevant information in all cases without any false cases).
As the number of health-care indicators continues to rise, the question of composite measure is on the agenda (Kelly & Hurst, 2006). Is it possible, desirable or both to construct overall measures of quality? A composite measure is a single measure that provides an overview of performance and quality. It is easier to communicate than the many single quality indicators, and points to the broader concept of quality, rather than to sub-dimensions and aspects. A comparison of composite measures between organizations can target organizations in need of special quality improvement. At the same time, it is an imminent feature of a quantitative analysis; the higher level of aggregation, the less information it provides. In practice, it means that serious flaws or shortcomings in health-care delivery may go under the radar of a composite measure, and that composite measures are not good at identifying sources of failures, and therefore of little use to actually improve the performance of the organization. The publication of composite measures is recommended only as long as it is followed with an explanation of the choice of indicators that are included, how they are transformed into the composite measure and the reason for the weighting structure that is used (Goodard & Jacobs, 2009). It has clearly been demonstrated that different methods of computing composite quality scores can lead to different conclusions being drawn (Reeves et al., 2007). The OECD quality indicator project chose to exclude composite measures for international comparison (Kelly & Hurst, 2006).
The purpose of quality indicators or performance measures are twofold: to promote accountability and to improve the performance of the health-care system (Smith, 2009). Assessing the quality of care may have different purposes for various stakeholders, and the purpose will influence what you are looking for. Policymakers need a confirmation from the health-care system: the citizen receive a good quality health care (outcome measures), and the money is well spent (structure and process measures). The health-care providers (health professionals and institutions) are interested in assessing the quality of care they provide and can influence (process measures), and the patients need to trust that the health-care system is providing the help they need when they need it, and that the quality of care is as good as possible (structure, process and outcome measures).
Measurement is a necessary condition if the health-care system is to be held accountable for its action and use of money. Policymakers who provide the funding of the health services need a tool to ensure that the money is well spent and that the quality of care is good, with the purpose of the indicators being accountability, in addition to ensuring public legitimacy and control. The providers of health care (institutions and organizations) need information to guide strategic decision making, and quality indicators may identify areas of care that need extra attention or resources. With regard to clinic quality, indicators are useful tools to guide quality improvement processes. As a basis for hospital choice or as a tool for trust building, indicators may also be used to communicate with the customers/patient. The transparency of the quality of care is important from the patient perspective, and will influence the expectation they have towards the health-care system.
Patient experiences is an important outcome variable in itself, and is also associated with patient safety and clinical effectiveness (Doyle, Lennox, & Bell, 2013). The evaluation of health-care quality should include the patient perspective, and patients can be included in evaluation of all core components of quality in the OECD quality indicator framework, including patient experiences, effectiveness and patient safety. International surveys of patient experiences with health services show that patients report several improvement areas (Schoen et al., 2011), thereby indicating the need for quality improvement. Examples of relevant resources include the CAHPS Improvement Guide (2014) literature on the effectiveness of patient-centered approaches to health care, and clinical guidelines and standards on the improvement of patient experiences (NICE, 2012).
In Norway, the Directorate of Health is responsible for a national quality indicator system for both primary and secondary care (Helsedirektoratet, 2013). The purposes of the national quality indicator system are to:
-
Provide a basis and incentive for health providers to continuously improve the quality and safety of their services;
-
Provide a basis for an individual choice of hospital;
-
A leadership tool for managers and owners;
-
Serve as a tool for policymakers and politicians in their evaluation and prioritizing of investments in health;
-
Inform the public/patient (transparency).
Improving quality of care
Even though selection mechanisms related to the public reporting of performance measures may cause improvements, the usual and most promising path from reports to improvement is some type of organizational change (Contandriopoulos, Champagne, & Denis, 2014). Since the publication of Crossing the quality chasm in 2001 (Institute of Medicine, 2001), the improvement science regarding quality and patient safety has been increasing in volume, and there are now several scientific journals dedicated to quality and quality improvement (e.g. BMJ Quality and Safety, the International Journal of Quality in Health Care).
Over the past three decades, there has been a shift from just ensuring quality to working with continuous quality improvement. During the last 10-15 years, three main approaches to quality improvement work are visible:
-
Systems for ensuring quality of the services (certification, systems of internal control, national quality indicators);
-
Clinically originated quality follow-up of one’s own practice, for example through professional clinical quality registries or clinical breakthrough learning groups;
-
Patient-oriented quality improvement through user experience surveys or involving patient groups or establishing patients’ committees.
For continuous quality improvement, various approaches need to be applied, and at different levels: the societal/political level, the organizational or institutional level, the clinical microsystems level (the interdisciplinary professional health-care team providing care to a particular group of patients) and at the individual patient level (Sosial- og helsedirektoratet, 2005).
The modern approach to quality and patient safety implies “systems thinking,” meaning that when they occur, poor quality or errors are made by competent, caring people who do their best in a flawed system that does not block errors from leading to harm (Wachter, 2012). But how about those physicians who for unknown reasons are not competent or responsible care providers (Bismark, Spittal, Gurrin, Ward, & Studdert, 2013; Light, 2003)? How can our need for a no-blame culture and focus on systems thinking be reconciled with the need for accountability? And how do we draw the line between the individual physician’s responsibility for quality of the care that he or she provides and the responsibility of the system, that is, the management of the hospital or the department?
Over the years, the health-care system has become much more complex than previously where there was only one physician, for example responsibility for the entire ward. Subsequent to this, the individual responsibility was huge, and the individual freedom to practice according to his or her own standards was undisputed. With the more complex health-care systems, a shift of responsibility towards the hospitals, and thus the managers of the hospitals, has developed (Hayes, Batalden, & Goldmann, 2015). Management must make sure that there are guidelines and procedures to ensure a sound professional practice, and health-care professionals must act as an employee to a much higher degree and follow the rules of the system. This may be perceived as being in conflict with the professional’s need for autonomy and thus job satisfaction. Batalden has stated that everybody in health care has two jobs; doing their job well, meaning with continuous updating of clinical knowledge and skills, and contributing to continuously improving the system in which one works (Batalden, Godfrey, & Nelson, 2007). However, the necessary quality improvement skills have not been an integrated part of the basic medical curriculum in Norway, and health professionals may thus feel insecure and uncomfortable with the needed systems thinking approach. The next generations of medical professionals will hopefully embrace the quality improvement science along with the medical science, and thus be empowered to improve the complex system they now work in. That might in turn lead to higher degree of job autonomy, satisfaction and through this higher quality of their work.
As part of the patient safety, systems thinking, a just culture has been defined as a culture in which frontline operators and others are not punished for actions, omissions or decisions taken by them that are commensurate with their experience and training, but where gross negligence, willful violations and destructive acts are not tolerated (Wachter, 2012). In order to bring about the best possible outcomes, this helps to build a culture that encourages coaching and honesty at all levels. It is not enough to be a knowledgeable and good physician or nurse. To be able to continue through the professional life to practice with high quality, some additional skills are needed, including the knowledge about the principles of quality improvement work, and how to promote a safe patient practice and an open patient safety culture, in which “no blame, no shame” is the leading principle. There is also a need to include knowledge about how to apply evidence-based medicine, as well as how to close the knowing-doing gap. A basic skill needed is to engage co-workers and leaders to join in on the quality improvement journey. The future health professional must be a team player and be a member of a team around the patient. A key question is whether the education of health-care professionals sufficiently includes these core competencies for the new obligations and the new professional roles. We also need role models to influence the newly educated in pursuing this proactive-, microsystem-oriented-, quality improvement- and patient safety-focused role.
It has not been rendered fair to focus on the individual physician’s contribution to the quality of care or the lack of quality of care, although there is now scientific evidence to support what everybody assumes, namely that the skills and quality of the performance of the physician are crucial for the outcome (Birkmeyer et al., 2013).
What is special about quality in health care?
In principle, the basic aspects of quality apply to health care just like they do to other services. Health care is a diverse and complex system, and quality is seen as the combined product of a high number of separate attributes or features, both measurable and non-measurable. These can be classified and organized in several ways, such as dimensions (Arah et al., 2006; Institute of Medicine, 2001; Rygh et al., 2010; Sosial- og helsedirektoratet, 2005).
Based on the relativity implicit in the relationship between outcome and requirements (ISO, 2005), quality is a dynamic dimension that varies over time and space. The media’s coverage of medicine and health plays an important part in the formation of expectations to health care. Diseases that occur frequently in the media are considered to be more common and more serious than diseases of comparable objective severity that receive less media attention. Such subjective perceptions of risk are essential in what psychologists call anchoring, a psychological heuristic that influences the way people intuitively assess probabilities, and thus also affect their expectations (Kahneman, 2011).
The difference between the hopes, wishes and expectations to health care on the one hand, and health care’s ability to fulfill these expectations in terms of preventing diseases, treating diseases and avoiding death and suffering on the other, can be called an expectation gap. An example of how such gaps are created is seen in the promotion of mass screening. Some people have come to believe that screening may prevent breast or cervical cancer, and not just detect it. Another challenge is the near automatic assumption that if a cancer arises soon after screening, it must have been missed through error (Wilson, 2000).
Even though it is hard to identify and define the outcome of health care, it is even harder to identify and define the expectations. Because “outcomes” of health care (e.g. survival) over the years have increased due to more effective treatments, expectations may have increased even faster. Expectations, e.g. as to diagnostic accuracy and sophisticated treatments, vary according to the level of care, thereby adding to the relativity of quality assessment. The same relativity is probably also related to economic resources. Moreover, expectations to health care are higher in wealthy than in poor societies, hence demanding a higher outcome.
Like other services, assessing the quality of health care also includes elements of subjectivity, which adds to the relativity based on differences in expectations and demands. The more or less identical consultation with a physician might be perceived rather differently by two similar patients, partially due to different priorities of measurable indicators such as waiting time or out-of-pocket payment.
Concluding remarks
A systematic review of improvement frameworks in health, education and social services identified seven conceptual approaches based on the Institute of Medicine’s recommendations, 32 based on Kaplan and Norton’s balanced scorecard, and ten based on Donabedian’s structure-process-outcome approach (Klassen et al., 2010). The review identified 16 quality concepts applicable across many settings, sectors and levels of application, concepts being equivalent to what we have termed dimensions in this manuscript. Consequently, there is a need to further standardize the quality approach in local, national and international health-care quality and quality assessment work.
We argue that the standardization work should use a health-care-specific approach to quality, for the following reasons:
-
Health-care services are special, as health care differs from other commodities in many respects. Health-care services include a variety of elements from brief consultations to long-term treatment plans. Emotional factors related to illness and disease play an important role in decision making that frequently must be done under uncertain conditions. There is a large asymmetry between “providers” and “customers” in terms of knowledge and experience than in most other “markets” in society. A quality concept tailor suited for health care is therefore needed. Insight into the complex nature of quality, understanding the aspects, dimensions and perspectives involved and the shared responsibility between organizations and individuals for quality improvement, as well as access to relevant and robust quality indicators, are all prerequisites for developing a better health-care system.
-
The conceptual approach should be acceptable by health-care workers since there have been several international standardizing efforts over the last few years (EU, OECD, Nordic Council of Ministers), but even these cross-national approaches vary. However, the conceptual models chosen in such projects indicate the importance of using health-care-specific quality approaches, not approaches from other public sectors or from the private sector. Regardless of the similarities or differences between health care and other services, a health-care-specific approach is probably more likely to receive legitimacy and acceptance from physicians and other health-care workers. This is of fundamental interest since physicians and other health-care workers are ultimately supposed to improve the quality of care.
The IOM and Donabedian approaches are quite similar and together provide a fruitful, coherent and health-care-specific approach to the quality of health care. We particularly emphasize the IOM’s definition and six dimensions (safe, effective, patient-centered, timely, efficient, equitable), and Donabedian’s point of varying dimensions depending on the health-care level being assessed and his structure-process-quality approach to assessing performance.
The more technical components of quality can be measured by a range of methods and indicators (Smith, 2009) but also by the patient perspective through patient-reported outcome measures (Fitzpatrick, Davey, Buxton, & Jones, 1998) and patient-reported safety measures (Bjertnaes, Skudal, Iversen, & Lindahl, 2013; McEachan et al., 2013). However, as Donabedian has stressed, the collected information about structures, processes and outcomes are not attributes of quality, but can be used to infer whether quality is good or not (Donabedian & Bashshur, 2003).
While quality evaluation have some elements of subjectivity and relativity, we stress that health care quality can be rather accurately defined, operationalized and measured. This can be achieved by combining the quality concept approach described above with state of the art quality measurement methods. The latter includes using more objective patient-reported experience instruments when including patients in quality evaluation, rather than subjective patient satisfaction questions, and the application of robust case-mix models to adjust for socio-demographic and other individual level variables. Furthermore, conjoint analysis can be applied to account for variation in attribute preferences, or alternatively completely patient defined instruments where patients themselves can define and prioritize attributes and then rate health care services on these.
Studies on the relationship between physicians’ working conditions and the quality of care should be based on an updated and comprehensive quality concept and scientifically robust quality indicators.
References
- Adair, C. E., Simpson, E., Casebeer, A. L., Birdsell, J. M., Hayden, K. A., & Lewis, S. (2006). Performance measurement in healthcare part II: state of the science findings by stage of the performance measurement process. Health Policy, 2(1), 56-78.
- Arah, O. A., Westert, G. P., Hurst, J., & Klazinga, N. S. (2006). A conceptual framework for the OECD Health Care Quality Indicators Project. International Journal for Quality in Health Care, 18 Suppl 1, 5-13. https://doi.org/10.1093/intqhc/mzl024
- Batalden, P. B., Godfrey, M. M., & Nelson, E. C. (2007). Quality by design: a clinical microsystems approach. San Francisco: Jossey-Bass.
- Birkmeyer, J. D., Finks, J. F., O'Reilly, A., Oerline, M., Carlin, A. M., Nunn, A. R., & Birkmeyer, N. J. (2013). Surgical skill and complication rates after bariatric surgery. New England Journal of Medicine, 369(15), 1434-1442. https://doi.org/10.1056/NEJMsa1300625
- Bismark, M. M., Spittal, M. J., Gurrin, L. C., Ward, M., & Studdert, D. M. (2013). Identification of doctors at risk of recurrent complaints: a national study of healthcare complaints in Australia. BMJ Quality & Safety, 22(7), 532-540. https://doi.org/10.1136/bmjqs-2012-001691
- Bjertnaes, O., Skudal, K. E., Iversen, H. H., & Lindahl, A. K. (2013). The Patient-Reported Incident in Hospital Instrument (PRIH-I): assessments of data quality, test-retest reliability and hospital-level reliability. BMJ Quality & Safety, 22(9), 743-751. https://doi.org/10.1136/bmjqs-2012-001756
- The CAHPS Improvement Guide. Retrieved 28. april 2014, from https://cahps.ahrq.gov/quality-improvement/improvement-guide/improvement-guide.html
- Contandriopoulos, D., Champagne, F., & Denis, J. L. (2014). The multiple causal pathways between performance measures' use and effects. Medical Care Research and Review, 71(1), 3-20. https://doi.org/10.1177/1077558713496320
- Council of Europe (1998). The development and implementation of quality improvement systems (QIS) in health care: recommendation No. R (97) 17 and explanatory memorandum. Retrieved from: http://www.coe.int/t/dg3/health/Source/Rec(97)17memo_en.doc
- Department of Health (1997). A first class service – quality in the new NHS. London: Department of Health.
- Donabedian, A. (1980). Explorations in quality assessment and monitoring Vol. 1. Ann Arbor, MI: Health Administration Press.
- Donabedian, A. (1988). The quality of care: how can it be assessed? JAMA, 260(12), 1743-1748. https://doi.org/10.1001/jama.1988.03410120089033
- Donabedian, A. (2005). Evaluating the quality of medical care. Milbank Quarterly, 83(4), 691-729. https://doi.org/10.1111/j.1468-0009.2005.00397.x
- Donabedian, A., & Bashshur, R. (2003). An introduction to quality assurance in health care. Oxford: Oxford University Press.
- Doyle, C., Lennox, L., & Bell, D. (2013). A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open, 3(1), e001570. https://doi.org/10.1136/bmjopen-2012-001570
- European Commission. Directorate-General Communication, European Commission. Directorate-General for Health and Consumer Protection, & European Opinion Research Group. (2010). Patient safety and quality of healthcare Special Eurobarometer 327. Brussels: TNS Opinion & Social.
- Fitzpatrick, R., Davey, C., Buxton, M. J., & Jones, D. R. (1998). Evaluating patient-based outcome measures for use in clinical trials. Health Technology Assessment, 2, 1-74.
- Gerteis, M., Edgman-Levitan, S., Daley, J., & Delbanco, T. L. (1993). Through the patient's eyes: understanding and promoting patient-centered care. San Francisco: Jossey-Bass.
- Goodard, M., & Jacobs, R. (2009). Using composite indicators to measure performance in health care. In P. Smith (Ed.), Performance measurement for health system improvement (pp. 339-368). Cambridge; New York: Cambridge University Press.
- Hayes, C. W., Batalden, P. B., & Goldmann, D. (2015). A 'work smarter, not harder' approach to improving healthcare quality. BMJ Quality & Safety, 24(2), 100-102. https://doi.org/10.1136/bmjqs-2014-003673
- Helsedirektoratet. (28. mai 2013). Hvorfor kvalitetsindikatorer? Retrieved 28. april 2014, from http://www.helsedirektoratet.no/kvalitet-planlegging/kvalitetsindikatorer/hvorfor-kvalitetsindikatorer/Sider/default.aspx
- Institute of Medicine. (1990). Medicare: A strategy for quality assurance, Vol.1. Washington, DC, National Academy Press.
- Institute of Medicine. (2001). Crossing the quality chasm: a new health system for the 21st century. Washington, D.C.: National Academy Press.
- Irvine, L., Elliott, L., Wallace, H., & Crombie, I. K. (2006). A review of major influences on current public health policy in developed countries in the second half of the 20th century. The journal of the Royal Society for the Promotion of Health, 126(2), 73-78. https://doi.org/10.1177/1466424006063182
- International Organization for Standardization. (2005). Quality management systems: Fundamentals and vocabulary (ISO 9000:2005) (Vol. TC 176//SC). Geneva: International Organization for Standardization.
- Jung, H. P., Wensing, M., Olesen, F., & Grol, R. (2002). Comparison of patients' and general practitioners' evaluations of general practice care. Quality & Safety in Health Care, 11, 315-319. https://doi.org/10.1136/qhc.11.4.315
- Kahneman, D. (2011). Thinking, fast and slow. New York: Farrar, Strauss and Giroux.
- Kelly, E., & Hurst, J. (2006). Health care quality indicators project: conceptual framework paper OECD Health Working Papers no. 23. Paris: OECD.
- Klassen, A., Miller, A., Anderson, N., Shen, J., Schiariti, V., & O'Donnell, M. (2010). Performance measurement and improvement frameworks in health, education and social services systems: a systematic review. International Journal for Quality in Health Care, 22(1), 44-69. https://doi.org/10.1093/intqhc/mzp057
- Lalonde, M., & Department of National Health and Welfare. (1974). A new perspective on the health of Canadians: a working document. Ottawa: Government of Canada. p. 77.
- Legido-Quigley, H., McKee, M., Nolte, E., & Glinos, I. (2008). Assuring the quality of health care in the European Union: A case for action. Copenhagen: WHO Regional Office for Europe. Observatory Service Series No. 12.
- Levine, R., Shore, K., Lubalin, J., Garfinkel, S., Hurtado, M., & Carman, K. (2012). Comparing physician and patient perceptions of quality in ambulatory care. International Journal for Quality in Health Care, 24, 348-356. https://doi.org/10.1093/intqhc/mzs023
- Light, D. (2003). Towards a new professionalism in medicine: quality, value and trust. Tidsskrift for den Norske Legeforening, 123(13-14), 13-14.
- Lohr, K. N. (1990a). Medicare: a strategy for quality assurance: volume I. Washington, D.C.: National Academy Press.
- Lohr, K. N. (1990b). Medicare: a strategy for quality assurance: volume II. Washington, D.C.: National Academy Press.
- McEachan, R. R., Lawton, R. J., O'Hara, J. K., Armitage, G., Giles, S., Parveen, S., & Wright, J. (2013). Developing a reliable and valid patient measure of safety in hospitals (PMOS): a validation study. BMJ Quality & Safety, 23(7), 565-573.
- McIntyre, D., Rogers, L., & Heier, E. (2001). Overview, history, and objectives of performance measurement. Health Care Financing Review, 22(3), 7-21.
- NICE. (2012). Patient experience in adult NHS services: improving the experience of care for people using adult NHS services NICE Clinical Guideline 138. London: National Clinical Guideline Centre.
- Quality (2014). In Merrian-Webster.com. Retrieved 28. april 2014, from http://www.merriam-webster.com/dictionary/quality
- Reeves, D., Campbell, S. M., Adams, J., Shekelle, P. G., Kontopantelis, E., & Roland, M. O. (2007). Combining multiple indicators of clinical quality: an evaluation of different analytic approaches. Medical Care, 45(6), 489-496. https://doi.org/10.1097/MLR.0b013e31803bb479
- Rygh, L. H., Helgeland, J., Braut, G. S., Bukholm, G., Fredheim, N., Frich, J. C., & Nguyen, K. N. (2010). Rapport fra Kunnskapssenteret nr 16-2010. Oslo: Nasjonalt kunnskapssenter for helsetjenesten.
- Schoen, C., Osborn, R., Squires, D., Doty, M., Pierson, R., & Applebaum, S. (2011). New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Affairs, 30, 2437-2448. https://doi.org/10.1377/hlthaff.2011.0923
- Sjetne, I. S., Bjertnaes, O. A., Olsen, R. V., Iversen, H. H., & Bukholm, G. (2011). The Generic Short Patient Experiences Questionnaire (GS-PEQ): identification of core items from a survey in Norway. BMC Health Services Research, 11, 88. https://doi.org/10.1186/1472-6963-11-88
- Smith, P. (2009). Performance measurement for health system improvement: experiences, challenges and prospects. Cambridge: Cambridge University Press.
- Sosial- og helsedirektoratet. (2005). -og bedre skal det bli!: nasjonal strategi for kvalitetsforbedring i Sosial- og helsetjenesten (2005-2015): til deg som leder og utøver IS-1162. Oslo: Sosial- og helsedirektoratet.
- Wachter, R. M. (2012). Understanding patient safety (2 ed.). New York: McGraw-Hill Medical.
- World Health Organization. (2000). The world health report 2000 : health systems: improving performance. Geneva: World Health Organization
- World Health Organization. (2006). Quality of care: a process for making strategic choices in health systems. Geneva: World Health Organization.
- Wilson, R. (2000). Screening for breast and cervical cancer as a common cause for litigation: a false negative result may be one of an irreducible minimum of errors. BMJ, 320(7246), 1352-1353. https://doi.org/10.1136/bmj.320.7246.1352