Thomas R. Konrad
Measures, Methods, and Models of Doctor Satisfaction: Future Research Challenges
Abstract: This paper outlines the way in which various concepts measuring doctor reactions to their jobs and careers (e.g., satisfaction, burnout, etc.) have been developed. The variety of measures, methods, and models reflect differing disciplinary and theoretical approaches and research traditions. In order to identify productive ways to advance the field, this paper presents a proposal for how multi-disciplinary, cross-national comparative research might be conducted to resolve some of the issues linking medical care organization, physicians' experiences, and patient outcomes. In seeking buy-in from stakeholders, researchers need to be cognizant that various ideologies and agendas shape the nature of the concerns that these interest groups (e.g., professional associations, clinical managers, payers, patient advocates, etc.) have about physician satisfaction, its precursors, and its consequences.
Keywords: Physician satisfaction; burnout; measurement; methodology; medical autonomy
Various concepts measuring doctor discontent (e.g., satisfaction, burnout, etc.) have been employed and measured. The measures, methods, and models used by academic researchers represent a wide variety of theoretical formulations and disciplinary approaches. I discuss the notion that variables operating at different levels of analysis have been posited as underlying factors accounting variation in physicians’ attitudes. These include health system organization and workplace variables, as well as different individual level life experiences and personalities. Patients’ clinical outcomes and satisfaction have been posited as being affected by doctor’s satisfaction. In order to identify productive ways to advance the field, this paper provides an example of how research has been conducted in the US and suggests how cross-national research might be conducted in response to the concerns that physicians, their employers, and their patients experience in the process of providing, overseeing, and receiving medical care.
The landscape of doctor disaffection: key concepts
Studies of physicians’ work have employed a number of concepts to study how doctors react to the situations in which they find themselves in their working lives: job and career satisfaction, burnout, stress, demoralization (Gabel, 2012), alienation (McKinlay & Marceau, 2011), physician well-being (Wallace & Lemaire, 2007), and resilience (Zwack & Schweitzer, 2013). Some discussions of these concepts characterize these phenomena as dispositional while at other times present them as situational (Maslach & Jackson, 2013). A wide range of psychological, social and cultural variables have been implicated in these discussions, and factors operating at various levels of analysis have been posited or observed as precursors, correlates, and consequences of physicians' perceptions and evaluations of their work and careers. Most observers seem to assume that individual personality and life history, training, and work experience variables affect the intensity and direction of the affective states which physicians report (McManus, Keeling, & Paice, 2004) but claim that more than psychological factors are involved (Gleichgerrcht & Decety, 2013). Numerous studies point to particular attributes of the local medical work settings as well as more general attributes of health care delivery systems as a source of stress, burnout, (Shanafelt et al., 2012), job dissatisfaction, or alienation (McKinlay & Marceau, 2011). A few observers posit medical school and residency as having consequences for subsequent disaffection, and more recently the advocates of continuing education have claimed a role in preventing burnout (Kjeldmand & Holmstrøm, 2008). Beyond this, a few have argued that underlying physician distress results to some extent from contradictory or unrealistic expectations embedded in the physician role itself (Friedberg, 2012; Gabel, 2012; Warde, Allen, & Gelberg, 1996).
Burnout
Burnout has its origins in field work with human service professionals and hence has special relevance to physicians, especially generalists and psychiatrists. Burnout has been associated with impaired job performance and poor health, including headaches, sleep disturbances, irritability, marital difficulties, fatigue, hypertension, anxiety, depression, myocardial infarction, and may contribute to alcoholism and drug addiction (Spickard, Gabbe, & Christensen, 2002). An extensive body of literature documents burnout in physician samples across a wide variety of specialties and populations. Three components of burnout include emotional exhaustion (EE: the depletion of emotional resources), depersonalization (DP: the development of a negative, callous and cynical attitude towards service recipients) and reduced personal accomplishment (PA: the tendency to evaluate one's work negatively, feelings of insufficiency and poor professional self-esteem) (Maslach & Jackson, 2013). Burnout develops over time (Houkes, Winants, Twellaar, & Verdonk, 2011), and some components (e.g., DP) may not be immediately cognitively accessible thus not reliably measured by survey self-report. Yet large physician surveys (Shanafelt et al., 2012) have used single items drawn from larger scales to represent EE and DP components (West, Dyrbye, Sloan, & Shanafelt, 2009). A single 5 statement item developed to represent the complex burnout concept (Schmoldt, Freeborn, & Klevit, 1994) has been validated (Rohland, Kruse, & Rohrer, 2004) and used in physician surveys; this index most closely correlates with the EE burnout subscale. A recent narrative review identified correlates of doctor burnout that elevate risk (Amoafo, Hanbali, Patel, & Singh, 2015) as demographic factors (i.e., female gender, younger age), workplace factors (i.e., heavy workloads and job dissatisfaction) and life situations (poor social support).
Measurement of job satisfaction
The US Tradition
The current framework for measurement of work satisfaction used in many US physician studies can be traced back to Herzberg’s mid 20th century studies of US workers which found distinct sources of work satisfaction and dissatisfaction (Herzberg, 1966). On the positive side, satisfaction resulted from intrinsically rewarding and intellectually stimulating “work itself,” and environments that granted recognition, fostered achievement, and supported advancement. Conversely, dissatisfaction was associated with “extrinsic” or “hygienic” factors such as poor supervision, restrictive company policies, suboptimal working conditions, contentious interpersonal relationships with colleagues and/or customers, and inadequate compensation. Herzberg asserted that minimal levels of these “hygienic” factors were required to prevent dissatisfaction with work, but removing these barriers did not necessarily increase satisfaction unless more satisfying elements were “intrinsic” to the job. This conceptual framework undergirded a widely used measurement tool called the Job Description Index (JDI) (Kinicki, McKee-Ryan, Schriesheim, & Carson, 2002).
This approach was applied to nursing studies (Stamps, Keuter, Byrne, Voell, & Larson, 2000), and physician specific items were developed for various components of job satisfaction (Stamps & Cruz, 1994). Stamps worked in hospital settings, while Lichtenstein (1984) focused on prisons, so the physician specific items developed for these tools concretely described work arrangements of doctors in those workplaces involving interdependent relationships with administrators, peers, and ancillary personnel. Unfortunately, these early scales failed to include items representing normative elements of professionalism discussed by medical sociologists, for example altruism, a service orientation, or putting patients’ interest first, that might be distinctive sources of gratification affecting physicians career or practice setting choices (Hafferty, 2006).
The UK tradition
In contrast to the JDI paradigm, most studies of physician job satisfaction in the UK and many other countries developed from a parallel industrial psychology tradition and measurement model (Warr, Cook, & Wall, 1979). These scales features multiple distinct intrinsic and extrinsic satisfaction facets, but subsequent adaptations for physicians simply omitted items that seemed not to make sense for this population. The most widely used summary scale uses 10 of the original 15 Warr items (Cooper, Rout, & Faragher, 1989; Rout & Rout, 1997). The five single item intrinsic factors are: freedom to choose your own method of working; amount of variety in your work; opportunities to use your abilities; recognition you get for good work; and amount of responsibility you are given. The four extrinsic factors are: your hours of work; your remuneration; physical working conditions; your colleagues and fellow workers. There is also a general satisfaction item: Taking everything into consideration, how do you feel about your work? Few studies analyze items separately. Some report the general satisfaction item alone, but most sum the 10 items to represent a global construct of physician job satisfaction, using Likert-type response options with a neutral midpoint anchored by "very dissatisfied" and "very satisfied." Varying numbers of response options, scoring methods, and satisfaction cutoff points have made it difficult to compare studies across settings or over time.
Despite its widespread use the last two decades, only one validation study of this scale has been conducted recently on a large population of Australian doctors (Hills, Joyce, & Humphreys, 2012), which found high level of internal consistency —but no support for differentiating intrinsic and extrinsic facets. Hills et al. (2012) suggest including other profession specific job-specific attributes in the scale, especially for physicians working in organizational settings. They also caution that a more inclusive, multi-factor instrument might be needed for in-depth, diagnostic approaches to job satisfaction, and concede that the scale’s brevity may have omitted important facets of job satisfaction in clinical medicine, limiting its capacity to discriminate between different levels of job satisfaction. The authors cautioned that single-item measures of global job satisfaction be may be biased because respondents may overstate levels of summary job satisfaction when not given the choice to answer specific items that would have required the choice of lower values.
It is interesting to note that the original Warr items omitted from physician versions of the scale describe elements of the work environment inconsistent with the notion of the solo practitioner (e.g., immediate supervisor, promotion opportunities, input into organizational policy, effectiveness of local management of the firm, and relationships between management and workers). As more physicians take on employee status and/or work in more tightly regulated environments (McKinlay & Marceau, 2002), these aspects of doctors’ work have come back into research designs either through the pathway of environmental descriptors or as additional facets of job satisfaction measures.
The Career Satisfaction Study Group
The Career Satisfaction Study Group (CSSG), established within the society of General Internal Medicine in the US, has conducted research over the last two decades largely dealing with the causes and consequences of low morale in the generalist or primary care physician sector. There is widespread concern among medical educators that a lack of interest in primary care careers by medical students would exacerbate an already growing shortage of these vital front line physicians in the US. Support for the three major projects described below has been garnered from public and private sources.
The Physician Worklife Study
One of the most extensive efforts to measure physician job satisfaction using the multi-faceted approach was the Physician Worklife Study (PWS) conducted in the US in the late 1990s by a multi-disciplinary, multi-institutional research team (Konrad et al., 1999; Linzer et al., 2000; McMurray et al., 1997; Williams et al., 1999). Information was gathered by examining open-ended responses from a 1988 survey of large group practice physicians (McMurray et al., 1997). Other items were gleaned from analyzing transcripts of six physician focus groups including ethnic minority and female physicians and those working with challenging populations. This source data confirmed the importance of relationships with patients, subordinates and physician peers, and of day-to-day practice environments, and identified distinctive issues for subgroups of physicians by gender, ethnicity, and practice type.
From this information an extensive item bank was developed and winnowed down in national surveys of US physicians (Konrad et al., 1999; Williams et al., 1999). Application of psychometric techniques yielded 10 facets; three dealt with resources: pay, clinical resources, and personal time; another three dealt with restrictions: autonomy, administration, and patient care issues; four facets dealt with relationships: physician colleagues, other clinical and administrative staff, patients, and the larger community. The survey also featured three 5-item global satisfaction scales measuring job, career, and specialty satisfaction. PWS adaptations and replications internationally have been successful with generally consistent pattern of positive relationships between facets and global measures, although somewhat different facets emerge in different countries. The Japanese adaptation added a prestige facet (Ozaki, Bito, & Matsumura, 2008); while a Swiss multi-faceted version identified five facets: patient care, burden, income-prestige, personal rewards, and professional relations and includes a single item global satisfaction measure (Bovier & Perneger, 2003).
Analyses of facet specific patterns of association with global measures suggest that there are multiple pathways to overall job satisfaction. The pattern of relationships between the various facets and global job satisfaction can differentiate different segments of the medical workforce. For example, global job satisfaction is more strongly associated with satisfaction with relationships with patients among primary care physicians that is the case for specialists, while medical specialists’ global job satisfaction is more closely correlated with satisfaction with other physician colleagues than is the case for primary care physicians (Linzer et al., 2000).
The MEMO study
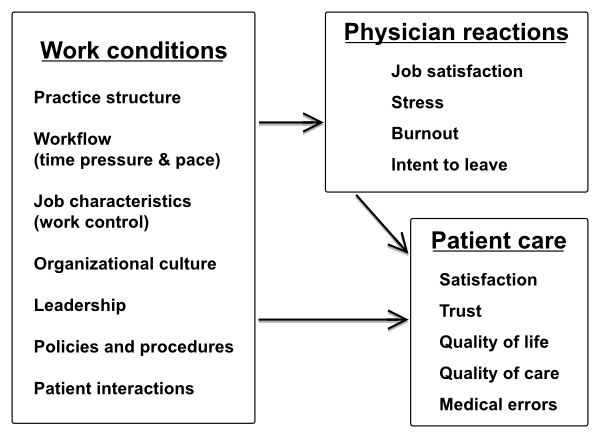
The MEMO study (Linzer et al., 2009) initiated and conducted by this study team of investigators, examined working conditions, physician reactions to those conditions, and health care quality at 119 ambulatory care clinics in the USA. The logic model is displayed in Figure 1.
Primary data collection employed site visits, direct observation in waiting rooms, interviews with clinic managers, physician surveys, lengthy abstractions of systematically selected patient records and patient surveys. Despite interesting descriptive findings, data analyses only partially supported the hypothesized model. There were strong associations between adverse working conditions and negative physician reactions (dissatisfaction, stress, burnout, and intention to leave practice) with some associations between adverse working conditions and health care quality and errors. Workflow (time pressure and a chaotic work pace), job characteristics (lack of work control), and poor organizational culture (e.g., lack of values alignment between staff and leadership) were strongly associated with adverse physician reactions. A few working conditions were inconsistently associated with poorer patient care, but adverse physician reactions, such as dissatisfaction, stress, and burnout, were not associated with poorer patient care.
One plausible interpretation of this array of findings is that physicians act as buffers between adverse work conditions and patient care—situations affect them strongly, but their reactions do not translate into lower quality care for their patients. The implications of this for physician health, mental health and well-being are worth contemplating. On the other hand, because adverse work conditions were strongly associated with intent to leave the practice, care could eventually suffer from interruptions brought on by the departure of physicians. Because turnover could not be measured within the observation period, it was impossible to assess its impact on continuity or quality in this sample, although there is other evidence that discontinuous care does in fact adversely affect patient outcomes over time (Konrad, Howard, Edwards, Ivanova, & Carey, 2005). The investigators also concluded that their findings may explain difficulties in recruiting and retaining generalists but leave open the question of whether adverse work conditions influence health care quality and safety.
The Healthy Workplace Study
The next phase of the CSSG research team’s activity, the Healthy Workplace Study (HWP) (Linzer et al., 2015), was an intervention aimed at making physician work more satisfying while improving patient care. With this dual aim in mind, the investigators chose to setup and implement a cluster randomized controlled trial with clinicians in 34 different sites in three different regions of the US. When they volunteered to enroll, clinicians provided a variety of baseline survey data collected from their staffs and quality indicators gleaned from the organization’s own medical records. The investigators hypothesized that changes in the workplace, initiated in response to feedback about clinician perceptions and performance, would result in decreased negative outcomes for clinicians and better care for their patients. The specific research question was: "Does receipt of baseline data on work conditions and targeted clinical interventions improve satisfaction, stress, burnout, and intent to leave practice?"
The intriguing aspect of this trial was that the “intervention” employed with the aim of increasing physician satisfaction and reducing burnout, was not prescribed by the investigators, but designed by the clinician subjects themselves and not primarily directed at individual physicians, but at entire primary care teams. Because the specific content of the intervention was not pre-specified by the investigators, the issue of treatment fidelity, that is, heterogeneity in the major treatment variable and limited control over the “dosage” and pace of the implementation, would seem problematic. The practice leadership in all “intervention” clinics received structured feedback in a two-page summary which profiled issues that practice team members themselves had identified as problems. Clinic staffs then met to design and put in place some kind of innovation that they thought would be effective in improving care for patients while making their own work lives more satisfying or at least less chaotic.
This approach makes sense, given that so many of the complaints of physicians, particularly in the US, are negative reactions to a perceived loss of autonomy due to external directives—clinical guidelines, performance standards, or burdensome paperwork, as noted by Casalino & Crosson (2015) in this special issue. In the Healthy Work Place study, investigators functioned like management consultants, suggesting options with some underlying evidence; but participating practitioners ultimately decided which elements they would incorporate in their own plans and took responsibility for implementation.
The study found that while stress was not affected by the intervention, sizeable reductions in clinician burnout and increases in job satisfaction were observed overall. Drilling down further, the research team concluded that efforts to improve communication or workflow were effective in lowering burnout and improving job satisfaction, and may have decreased intention to leave. The implementation of quality improvement projects driven by clinician concerns also reduced burnout.
This research demonstrates that engaging medical staffs in an effort to empower themselves to alter workplace factors and clinical regimens of care can yield positive results. In sociological terms, this means identifying structural barriers in the work place and activating collective agency to overcome them. Although the impacts of these interventions on patient perceptions and clinical care are still being examined (Linzer, personal communication, April 2, 2015), it is clear that the Healthy Work Place approach has promise. It also suggests that using a sociological lens and developing a teamwork perspective may be an important and underappreciated factor in the study of physician job satisfaction and the improvement of care in real world settings.
Lessons from the CSSG experience
The three projects reported by this team illustrate what may be required to advance efforts in this field. First, the focus of the research is on a question that major segments of the medical profession and medical educators are concerned about—indeed, the question is about their survival as a vital segment of the medical profession. Secondly, a variety of disciplines—physicians, psychometricians, sociologists, epidemiologists, management—guided the research. Finally, active engagement and buy-in of the subjects in the design and implementation of the research was critical to the success of the enterprise.
Next steps
Cross national comparative study
So where do we go from here? It is not too soon for an international collaborative study linking physicians’ work experiences and attitudes to the structure and culture of their workplaces. Such a project would examine how such factors might affect the outcomes experienced by their patients and perhaps even launch efforts to improve work lives of physicians. This undertaking would require careful planning, involving a variety of stakeholders by convincing them to make substantial long range commitments to the project as sponsors and/or subjects. Such a project would require identifying many stakeholders in different countries, fully engaging them and offering them options to participate in different components of the study phased in over a lengthy time period. To secure buy-in from key stakeholders, the potential benefits of carefully collected data-based cross-national studies should be clearly defined and made obvious to all including not only key physician groups and medical educators, but political figures and health policy makers in different countries. Both the strengths and limitations of proactive and deliberately initiated data collection should be well defined. The interests of various stakeholders in obtaining strategic but objective information about the physician workforce should be articulated. Such a process might serve as an effective counterweight to superficial comparative studies of health policy that have led to facile generalizations (Marmor, Freeman, & Okma, 2005).
The ideal cross-national comparative study would involve enough countries and systems to broadly represent major variations in the design and financing of health systems as well important variations in employment situations of physicians within those systems (e.g., small vs. large settings, self-employment vs. employee status, inpatient vs. outpatient focus, various patient populations, public vs. private sector, etc.). It might be best to initially target generalists to best address the questions raised in this volume. The overall study design would require linking clinic and community level characteristics to physicians working in each setting as well as to patients being served there. Ideally, a panel design would involve clinics as the primary sampling unit rather than individual practitioners. If individual patient-physician linkage is possible, some consistent, credible, readily implementable rules would be required linking a set of patients that is large enough to generalize to each individual physician assumed to be their doctor. Failing this, patients should be linked to a small stable team of practitioners virtually all of whom should be study participants. Ideally the same set of “process indicators” or “tracer conditions” would be used to assess “quality” outcomes across nations. But this might not inevitably be the case, assuming a statistical distribution of patient outcomes could generate enough interval or ordinal scale data that would be sensitive enough to detect “clinically important” differences as benchmarked against national averages or clinical standards. Patient perception and/or satisfaction data would also be useful. Based on the experience with the MEMO study and the HWP in the US, this type of study design is feasible, but challenging even in one country.
Multifaceted measurement of job satisfaction is recommended not only for its scientific validity, but also because it is likely to build and sustain commitment across countries as well as among different types of stakeholders. This is so because their distinctive concerns are likely to be addressed by more nuanced descriptions inherently possible with multifaceted measurements. Existing measures aimed at the clinic staff as well as the physicians should probably be the starting point for instrument development. Much of the instrumentation could include validated survey instruments such as the recent RAND/AMA study (Crosson and Casalino, 2015) but some primary scale development could be done. Physician surveys should use uniform wording for core clinical tasks, patient physician relationships, demographics, educational, and health history information. Yet, to make surveys interpretable by physician participants in different systems, country-specific modules should be developed using locally meaningful terminology to describe financing, payment, and organizational issues physicians deal with routinely and can meaningfully evaluate from their own perspective. However, prior to the conduct of the study itself, investigators should agree about how to set up and describe any statistical comparisons involving these system-related variables so valid comparative conclusions can be drawn, thus minimizing ad hoc assumptions or post hoc comparisons.
Given this broad outline, some strategic decisions would need to be made. Probably not every participating country needs to be engaged in both the clinic/physician and the patient care outcomes study phases; relatively few might opt for involvement in any intervention phase. Obviously the second and third phases are likely to be more time-consuming, difficult and risky for participants and relatively difficult to implement without extensive on the ground engagement of a study staff. Perhaps existing national or regional practice networks (Soler et al., 2008; Soler, Yaman, & Esteva, 2007) could be employed in such an enterprise. Creative data collection strategies such as the overlapping questionnaire design approach so helpful in longitudinal panel studies of Norwegian doctors (Aasland, Olff, Falkum, Schweder, & Ursin, 1997; Rosta & Aasland, 2014) could be applied in cross sectional and longitudinal design.
Sociological perspectives and challenges
Job satisfaction, career satisfaction, and life satisfaction have often been conflated in editorials and policy discussions (Linn, Yager, Cope, & Leake, 1986). The linkage between job and career satisfaction and life satisfaction is especially important for physicians, because their professional role has traditionally been so central to their self-concept, so that other roles (kinship, community) may seem peripheral. Paradoxically the consuming centrality of the physician role in the individual’s self at work may drive physicians to perfectionist attempts to adhere to impossible standards. Negative feelings doctors have when finding themselves failing in these efforts may reverberate back into their attitudes with life in general. This in turn might lead them to experience more distress at work which in the extreme manifests as occupational impairment (Simpson & Grant, 1991).
The most comprehensive measurements of physician job satisfaction have been conceptualized as multifaceted, even if these facets are measured with single items and only summary scores reported. Not surprisingly, these kinds of survey instruments are more popular with the researchers who produce them than with the physicians at whom they are aimed. Social scientists must rely on the good will of their subjects to successfully collect data from them; yet if doctors’ chief complaints are about burdensome documentation, survey intensive research approaches may be seen by physicians as part of the problem rather than part of the solution. There are significant costs involved in obtaining a comprehensive picture of the relationships between different aspects of medical work. Although many researchers pay lip service to the idea that job satisfaction is a multifaceted concept, they find themselves forced to truncate scales or conflate their measurement strategy to a single item or a single scale. Reducing the complexity of data collection runs the risk of distorting the representation of the actual phenomena being studied and misidentifying the kinds of actions that might be taken to ameliorate problems of physicians and their patients. If job satisfaction is multi-faceted, a nuanced approach should assess distinctive antecedents, correlates, and consequences of its various facets. The work of most physicians is quite heterogeneous, and some specific mix of the intellectually challenging, emotionally satisfying, and socially useful aspects of tasks involved in the delivery of health care is likely to provide gratification to most doctors. It is likely that particular combinations of certain values and rewards vary systematically if subtly within different segments of the medical workforce and may also vary across countries to the extent that societal and cultural expectations about the physician role may also subtly vary across systems.
The theoretical frameworks of life course sociology or the social psychology of adult development have been employed only rarely in physician satisfaction research and these streams of theory and research could enrich the field considerably. The use of longitudinal panels of physicians is critical to disentangling the effects of historical changes, cohort composition and entry, and individual biographical events on how physicians view their work and career as well linking these phenomena to antecedents and outcomes. Only a few studies have noted variability over the life course or career stage in sources of stress identified. One inquiry into physicians’ sources of stress identified four factors: patient relationships, business/financial issues, time pressures, and competence concerns (Simpson & Grant, 1991). Not surprisingly, concerns about competence were important sources of job stress among young physicians, but diminished among older ones. Similar patterns of variation over the life course were found linking anxiety due to clinical uncertainty and apprehension about negative outcomes (Bovier & Perneger, 2007; Dyrbye et al., 2013). Such studies are difficult to conduct unless longitudinal study designs are employed, but repeated cross-sectional studies using similar instrumentation can be very useful if not definitive in disentangling effects of age, period and cohort in physician attitudes. Firth-Cozens & Greenhalgh (Firth-Cozens & Greenhalgh, 1997) describe the link between stress and untoward outcomes and build a powerful case that physicians believe that such a causal link exists in their own work. Similarly, an 11 year follow-up of a cohort of students transitioning to work (Firth-Cozens, 2001) suggests job dissatisfaction may affect patient outcomes (including patient satisfaction and compliance with recommended regimens of care) through the stress pathway.
Concluding observations
A recent systematic review (Scheepers, Boerebach, Arah, Heineman, & Lombarts, 2015) identified 18 studies relating occupational well-being of physicians to quality of care. Occupational well-being was defined as a positive experience with or evaluation of one’s work involving satisfaction, commitment, involvement, or engagement. “Quality” was broadly and inclusively defined, using a variety of measurement approaches. The authors reported that patients of physicians with higher levels of occupational well-being were more satisfied with their treatment and were more likely to follow treatment recommendations. They noted that study designs were not particularly strong, and that results involving the technical aspects of patient care (i.e., “process” measures) were conflicting. As were four studies where the outcome was “medical error,” where two studies found a relationship and two did not. They also found that higher levels of occupational well-being did not prevent physicians from delivering superfluous medical care, that is, care which is not necessary according to the most recent standards (Grol et al., 1985). It is worth noting that in most studies with quality outcomes measured independently of the physician, for example using record reviews or aggregated patient self-report of health, no relationship between quality and satisfaction was found (Deshpande & Deshpande, 2014; Linzer et al., 2009; Utsugi-Ozaki et al., 2009), whereas the bulk of the studies that support the relationship involve physician self-reports of one or more quality indicators. Although physicians, like anyone, likely exhibit bias in judging the quality of their own work (Davis et al., 2006), this subjective correlation between quality and satisfaction is not insignificant. Nonetheless, the take away message from Scheepers et al.’s review is clear: “…future research on occupational well-being could benefit from standardized measures on technical aspects of patient care” (2015, “Discussion”, para. 5).
Angerer and Weigl (2015), in this special issue, address the same set of questions that Scheepers et al. do using a framework that is quite similar. Although the specific articles chosen for intensive review by Angerer and Weigl only slightly overlap with those chosen by the other research team, the conclusions they reach are quite similar as are the recommendations they make for further research. The fact that two highly competent research teams independently come to quite similar conclusions by applying rigorous methods to somewhat different bodies of evidence suggests that there is indeed something important going on here. Both groups advocate for better designed and more focused research, which might include longitudinal, comparative, and interventional approaches to resolve some of the outstanding issues. I would add to these discussions that the next logical step might address larger questions about how structural features in the various national health systems might impede or enhance the quality of work for physicians and the quality of care for their patients.
Certain key questions remain. What is the relationship between physician satisfaction and quality of care? Is physician satisfaction a determinant of or marker for quality? Conversely, is physician dissatisfaction a “red flag” for poor quality care? Is there no relationship at all? Empirical evidence has been found for all of these propositions, and numerous measurement challenges for both concepts remain. Relationships may be conditional on as yet untheorized and unmeasured mediating or modifying variables. There is widespread recognition that the measurement of quality is complex and multifaceted. My argument here has been is that the measurement of physician satisfaction and dissatisfaction is no less complex, and that complexity should be explored not ignored.
Just as there are “origin myths” about the medical profession (Dingwall, 2014), I would argue that there are also “operating myths” that surround the notion of the healer and that are fused into the modern self-concept of the physician. One contemporary metaphor is the physician as an airline pilot or race car driver—the strong, confident individual flying solo with a supporting team (Aasland, 2015). This myth, which resonates particularly in the American context, has promoted an unrealistic ethic of heroic but isolated individualism—that may have contributed to the problem of “burnout” and discontent. But it may have had an unexpected positive side as well. This analogy has facilitated the health care industry’s adoption of the airline industry’s programmatic efforts to implement safety regimes, and in the process has made such an emphasis on safety more palatable to physicians. The parallel works to some extent because physicians, particularly those in the surgical specialties, have come to recognize that that using a checklist does not threaten the autonomy of the pilot (Gawande & Lloyd, 2010) and having additional professionals in the cockpit certainly makes for increased patient safety.
I would argue that one theme of this collection of essays is about another operating myth of the medical profession. The widespread testimony of physicians that their own emotional states, however labeled, have a significant negative effect on their patients does not constitute sufficient scientific evidence to assent to the truth of the proposition that doctor discontent causes poor quality care or affects the health outcomes of the patients under their care. This proposition may not be true in the literal sense, and has proved to be difficult to empirically demonstrate in a scientifically credible or broadly generalizable manner. Yet it may be prudent to conclude that physicians’ belief in this link may be salutary after all.
The answer to the question: “Would you want care from a discontented doctor?” (Casalino & Crosson, 2015) may not be so obvious after all. The best response is: It depends on the source of that discontent and the consequences likely to flow given that particular physician’s pattern of life choices and experiences. If we discern that discontent takes the form of paralyzing uncertainty, demoralization, or the classic symptoms of burnout, most would avoid this doctor. On the other hand, if discontent signals a conscientiousness motivating the doctor to take action to improve his or her clinical competence, enhance his or her compassion, or improve care not only for his or her patients, but for the whole community, this just might be the doctor that most would seek out for care.
References
- Aasland, O. G. (2015). Healthy doctors—sick medicine. Professions and Professionalism, 5(1). https://doi.org/10.7577/pp.989
- Aasland, O. G., Olff, M., Falkum, E., Schweder, T., & Ursin, H. (1997). Health complaints and job stress in norwegian physicians: The use of an overlapping questionnaire design. Social Science & Medicine, 45(11), 1615-1629. https://doi.org/10.1016/S0277-9536%2897%2900093-2
- Amoafo, E., Hanbali, N., Patel, A., & Singh, P. (2015). What are the significant factors associated with burnout in doctors? Occupational Medicine, 65(2), 117-121. https://doi.org/10.1093/occmed/kqu144
- Angerer, P., & Weigl, M. (2015). Physicians' psychosocial work conditions and quality of care: a literature review. Professions and Professionalism, 5(1). https://doi.org/10.7577/pp.960%20%20
- Bovier, P. A., & Perneger, T. V. (2007). Stress from uncertainty from graduation to retirement—a population-based study of swiss physicians. Journal of General Internal Medicine, 22(5), 632-638. https://doi.org/10.1007/s11606-007-0159-7
- Bovier, P. A., & Perneger, T. V. (2003). Predictors of work satisfaction among physicians. European Journal of Public Health, 13(4), 299-305. https://doi.org/10.1093/eurpub/13.4.299
- Byrne, E., Keuter, K., Voell, J., & Larson, E. (2000). Nurses' job satisfaction and organizational climate in a dynamic work environment. Applied Nursing Research, 13(1), 46-49. https://doi.org/10.1016/S0897-1897(00)80018-X
- Casalino, L. P., & Crosson, F. J. (2015). Physician satisfaction and physician well-being: should anyone care? Professions and Professionalism, 5(1). https://doi.org/10.7577/pp.954
- Cooper, C. L., Rout, U., & Faragher, B. (1989). Mental health, job satisfaction, and job stress among general practitioners. BMJ: British Medical Journal (International Edition), 298(6670), 366-370. https://doi.org/10.1136/bmj.298.6670.366
- Davis, D. A., Mazmanian, P. E., Fordis, M., Van, R., Thorpe, K. E., & Perrier, L. (2006). Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. Journal of the American Medical Association, 296(9), 1094-1102. https://doi.org/10.1001/jama.296.9.1094
- Deshpande, S. P., & Deshpande, S. S. (2014). Antecedents of care by physicians. The Health Care Manager, 33(1), 38-44. https://doi.org/10.1097/01.HCM.0000440622.39514.44
- Dingwall, R. (2014). Physician discontent and the changing context of professional work. Paper prepared for the symposium Doctors’ professional satisfaction, quality of care, and the governance of health care organizations. Oslo, Norway, June 2-3, 2014.
- Dyrbye, L. N., Varkey, P., Boone, S. L., Satele, D. V., Sloan, J. A., & Shanafelt, T. D. (2013). Physician satisfaction and burnout at different career stages. Mayo Clinic Proceedings, 88(12), 1358-1367. https://doi.org/10.1016/j.mayocp.2013.07.016
- Firth-Cozens, J. (2001). Interventions to improve physicians’ well-being and patient care. Social Science & Medicine, 52(2), 215-222. https://doi.org/10.1016/S0277-9536%2800%2900221-5
- Firth-Cozens, J., & Greenhalgh, J. (1997). Doctors' perceptions of the links between stress and lowered clinical care. Social Science & Medicine, 44(7), 1017-1022. https://doi.org/10.1016/S0277-9536%2896%2900227-4
- Friedberg, M. W. (2012). The potential impact of the medical home on job satisfaction in primary care. Archives of Internal Medicine, 172(1), 31-32. https://doi.org/10.1001/archinternmed.2011.579
- Gabel, S. (2012). Demoralization: A precursor to physician burnout? American Family Physician, 86(9), 861-862.
- Gawande, A., & Lloyd, J. B. (2010). The checklist manifesto: How to get things right. New York: Metropolitan Books.
- Gleichgerrcht, E., & Decety, J. (2013). Empathy in clinical practice: How individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One, 8(4), e61526. https://doi.org/10.1371/journal.pone.0061526
- Grol, R., Mokkink, H., Smits, A., van, J., Beek, M., Mesker, P., & Mesker-Niesten, J. (1985). Work satisfaction of general practitioners and the quality of patient care. Family Practice, 2(3), 128-135. https://doi.org/10.1093/fampra/2.3.128
- Hafferty, F. W. (2006). Definitions of professionalism: A search for meaning and identity. Clinical Orthopaedics and Related Research, 449, 193-204.. https://doi.org/10.1093/fampra/2.3.128
- Herzberg, F. (1966). Work and the nature of man. Cleveland: World Pub. Co.
- Hills, D., Joyce, C., & Humphreys, J. (2012). Validation of a job satisfaction scale in the australian clinical medical workforce. Evaluation & the Health Professions, 35(1), 47-76. https://doi.org/10.1177/0163278710397339
- Houkes, I., Winants, Y., Twellaar, M., & Verdonk, P. (2011). Development of burnout over time and the causal order of the three dimensions of burnout among male and female GPs. A three-wave panel study. BMC Public Health, 11(1), 240. https://doi.org/10.1186/1471-2458-11-240
- Kinicki, A. J., McKee-Ryan, F. M., Schriesheim, C. A., & Carson, K. P. (2002). Assessing the construct validity of the job descriptive index: A review and meta-analysis. Journal of Applied Psychology, 87(1), 14. https://doi.org/10.1037/0021-9010.87.1.14
- Kjeldmand, D., & Holmstrøm, I. (2008). Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Annals of Family Medicine, 6(2), 138-145. https://doi.org/10.1370/afm.813
- Konrad, T. R., Howard, D. L., Edwards, L. J., Ivanova, A., & Carey, T. S. (2005). Physician-patient racial concordance, continuity of care, and patterns of care for hypertension. American Journal of Public Health, 95(12), 2186-2190. https://doi.org/10.2105/AJPH.2004.046177
- Konrad, T. R., Williams, E. S., Linzer, M., McMurray, J., Pathman, D. E., Gerrity, M., Schwartz, M. D., Scheckler, W. E., Van Kirk, J., Rhodes, E., & Douglas, J. (1999). Measuring physician job satisfaction in a changing workplace and a challenging environment. Medical Care, 37(11), 1174-1182. https://doi.org/10.1097/00005650-199911000-00010
- Lichtenstein, R. (1984). Measuring the job satisfaction of physicians in organized settings. Medical Care, 22(1), 56-68. https://doi.org/10.1097/00005650-198401000-00005
- Linn, L. S., Yager, J., Cope, D. W., & Leake, B. (1986). Factors associated with life satisfaction among practicing internists. Medical Care, 24(9), 830-837. https://doi.org/10.1097/00005650-198609000-00004
- Linzer, M., Manwell, L. B., Williams, E. S., Bobula, J. A., Brown, R. L., Varkey, A. B., Man, B., McMurray, J. E., Maguire, A., Horner-Ibler, B., & Schwartz, M. D. (2009). Working conditions in primary care: Physician reactions and care quality. Annals of Internal Medicine, 151(1), 28-36. https://doi.org/10.7326/0003-4819-151-1-200907070-00006
- Linzer, M., Poplau, S., Grossman, E., Varkey, A., Yale, S., Williams, E., Hicks, L., Brown, R. L., Wallock, J., Kohnhorst, D., & Barbouche, M. (2015). A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: Results from the healthy work place (HWP) study. Journal of General Internal Medicine, 1-7. https://doi.org/10.1007/s11606-015-3235-4
- Linzer, M., Konrad, T. R., Douglas, J., McMurray, J. E., Pathman, D. E., Williams, E. S., Schwartz, M. D., Gerrity, M., Scheckler, W., Rhodes, E., & Society of General Internal Medicine (SGIM) Career Satisfaction Study Group (CSSG). (2000). Managed care, time pressure, and physician job satisfaction: Results from the physician worklife. JGIM: Journal of General Internal Medicine, 15(7), 441-450. https://doi.org/10.1046/j.1525-1497.2000.05239.x
- Marmor, T., Freeman, R., & Okma, K. (2005). Comparative perspectives and policy learning in the world of health care. Journal of Comparative Policy Analysis: Research and Practice, 7(4), 331-348. https://doi.org/10.1080/13876980500319253
- Maslach, C., & Jackson, S. E. (2013). Burnout in the health professions: A social psychological analysis. In G. S. Sanders & J. Suls (Eds.), The Social Psychology of Health and Illness (pp. 222-254). Hillsdale, NJ: Lawrence Earlbaum Associates.
- McKinlay, J. B., & Marceau, L. D. (2002). The end of the golden age of doctoring. International Journal of Health Services, 32(2), 379-416. https://doi.org/10.2190/JL1D-21BG-PK2N-J0KD
- McKinlay, J. B., & Marceau, L. D. (2011). New wine in an old bottle: Does alienation provide an explanation of the origins of physician discontent? International Journal of Health Services, 41(2), 301-335. https://doi.org/10.2190/HS.41.2.g
- McManus, I. C., Keeling, A., & Paice, E. (2004). Stress, burnout and doctors' attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Medicine, 2, 29. https://doi.org/10.1186/1741-7015-2-29
- McMurray, J. E., Williams, E., Schwartz, M. D., Douglas, J., Van, J., Konrad, T. R., Gerrity, M., Bigby, J. A., Linzer, M., & SGIM Career Satisfaction Study Group (CSSG). (1997). Physician job satisfaction: Developing a model using qualitative data. Journal of General Internal Medicine, 12(11), 711-714. https://doi.org/10.1046/j.1525-1497.1997.07145.x
- Ozaki, M., Bito, S., & Matsumura, S. (2008). Developing a japanese hospital physician satisfaction scale. International Journal of Health Care Quality Assurance, 21(5), 517-528. https://doi.org/10.1108/09526860810890486
- Rohland, B. M., Kruse, G. R., & Rohrer, J. E. (2004). Validation of a single‐item measure of burnout against the maslach burnout inventory among physicians. Stress and Health, 20(2), 75-79. https://doi.org/10.1002/smi.1002
- Rosta, J., & Aasland, O. G. (2014). Correction: Changes in the lifetime prevalence of suicidal feelings and thoughts among norwegian doctors from 2000 to 2010: A longitudinal study based on national samples. BMC Psychiatry, 14(1), 1. https://doi.org/10.1186/1471-244X-14-1
- Rout, U., & Rout, J. K. (1997). A comparative study on occupational stress, job satisfaction and mental health in british general practitioners and canadian family physicians. Psychology, Health & Medicine, 2(2), 181-190. https://doi.org/10.1080/13548509708400575
- Scheepers, R. A., Boerebach, B. C., Arah, O. A., Heineman, M. J., & Lombarts, K. M. (2015). A systematic review of the impact of physicians’ occupational well-being on the quality of patient care. International Journal of Behavioral Medicine,, 1-16. https://doi.org/10.1007/s12529-015-9473-3
- Schmoldt, R. A., Freeborn, D. K., & Klevit, H. D. (1994). Physician burnout: Recommendations for HMO managers. HMO Practice / HMO Group, 8(2), 58-63.
- Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., West, C. P., Sloan, J., & Oreskovich, M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
- Simpson, L. A., & Grant, L. (1991). Sources and magnitude of job stress among physicians. Journal of Behavioral Medicine, 14(1), 27-42. https://doi.org/10.1007/BF00844766
- Soler, J. K., Yaman, H., Esteva, M., Dobbs, F., Asenova, R. S., Katic, M., Ožvačić, Z, Desgranges, J. P., Moreau, A., Lionis, C., Kotányi, P., Carelli, F., Nowak, P. R., de Aguiar Sá Azeredo, Z., Marklund, E., Churchill, D., Ungan, M., & European General Practice Research Network Burnout Study Group. (2008). Burnout in european family doctors: The EGPRN study. Family Practice, 25(4), 245-265. https://doi.org/10.1093/fampra/cmn038
- Soler, J. K., Yaman, H., & Esteva, M. (2007). Burnout in european general practice and family medicine. Social Behavior and Personality, 35(8), 1149-1150. https://doi.org/10.2224/sbp.2007.35.8.1149
- Spickard, A. Jr., Gabbe, S. G., & Christensen, J. F. (2002). Mid-career burnout in generalist and specialist physicians. Journal of the American Medical Association, 288(12), 1447-1450. https://doi.org/10.1001/jama.288.12.1447
- Stamps, P. L., & Cruz, N. T. (1994). Issues in physician satisfaction: New perspectives. Arbor, MI: Health Administration Press.
- Utsugi-Ozaki, M., Bito, S., Matsumura, S., Hayashino, Y., Fukuhara, S., & MEMO-J, Group. (2009). Physician job satisfaction and quality of care among hospital employed physicians in japan. Journal of General Internal Medicine, 24(3), 387-392. https://doi.org/10.1007/s11606-008-0886-4
- Wallace, J. E., & Lemaire, J. (2007). On physician well being—you’ll get by with a little help from your friends. Social Science & Medicine, 64(12), 2565-2577. https://doi.org/10.1016/j.socscimed.2007.03.016
- Warde, C., Allen, W., & Gelberg, L. (1996). Physician role conflict and resulting career changes. Journal of General Internal Medicine, 11(12), 729-735. https://doi.org/10.1007/BF02598986
- Warr, P., Cook, J., & Wall, T. (1979). Scales for the measurement of some work attitudes and aspects of psychological well‐being. Journal of Occupational Psychology, 52(2), 129-148. https://doi.org/10.1111/j.2044-8325.1979.tb00448.x
- West, C. P., Dyrbye, L. N., Sloan, J. A., & Shanafelt, T. D. (2009). Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. Journal of General Internal Medicine, 24(12), 1318-1321. https://doi.org/10.1007/s11606-009-1129-z
- Williams, E. S., Konrad, T. R., Linzer, M., McMurray, J., Pathman, D. E., Gerrity, M., Schwartz, M. D., Scheckler, W. E., Van Kirk, J., Rhodes, E., & Douglas, J. (1999). Refining the measurement of physician job satisfaction: Results from the physician worklife survey. SGIM career satisfaction study group. society of general internal medicine. Medical Care, 37(11), 1140-1154. https://doi.org/10.1097/00005650-199911000-00006
- Zwack, J., & Schweitzer, J. (2013). If every fifth physician is affected by burnout, what about the other four? resilience strategies of experienced physicians. Academic Medicine, 88(3), 382-389. https://doi.org/10.1097/ACM.0b013e318281696b