Lawrence P. Casalino and Francis J. Crosson
Physician Satisfaction and Physician Well-Being: Should Anyone Care?
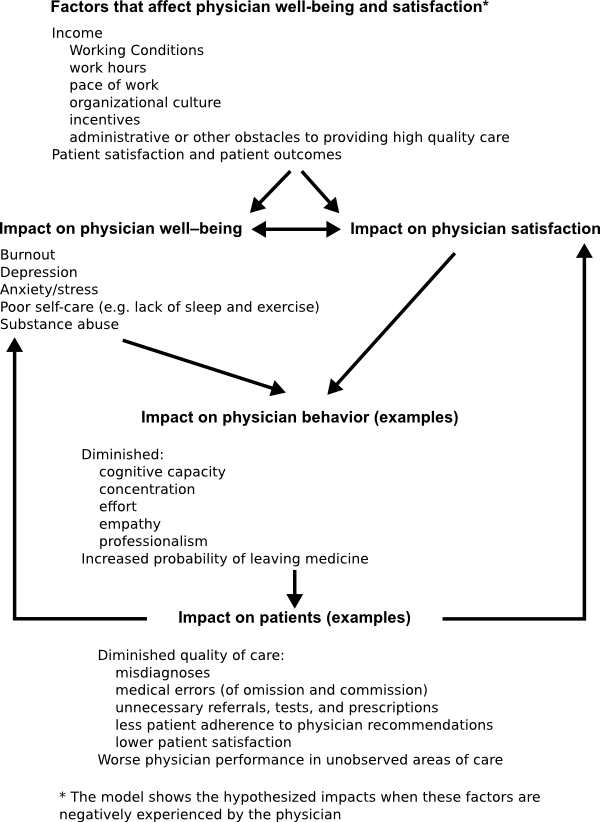
Abstract: We present a model of hypothesized relationships between physician satisfaction, physician well-being and the quality of care, in addition to a review of relevant literature. The model suggests that physicians who are stressed, burned out, depressed, and/or have poor self-care are more likely to be dissatisfied, and vice-versa. Both poor physician well-being and physician dissatisfaction are hypothesized to lead to diminished physician concentration, effort, empathy, and professionalism. This results in misdiagnoses and other medical errors, a higher rate of inappropriate referrals and prescriptions, lower patient satisfaction and adherence to physician recommendations, and worse physician performance in areas not observed by others. Research to date largely supports the model, but high quality studies are few. Research should include studies that are prospective, larger, and have a stronger analytic design, ideally including difference in differences analyses comparing quality of care for patients of physicians who become dissatisfied to those who remain satisfied, and vice versa.
Keywords: physician satisfaction; physician dissatisfaction; quality of care; physician well-being; physician burnout
It seems obvious that patients would prefer that their physician not be depressed, burned out, sleep-deprived, or addicted to drugs or alcohol. But in addition, it seems likely that patients would prefer their physician to be reasonably satisfied with his or her work. What would you say if you—the reader—were asked “Would you willingly consult a physician who is very dissatisfied with his or her work?” What would go through your mind? Will the physician care about you? Will she make you feel uncomfortable? Will she order the right tests? Will she be conscientious about details? Will she make the right diagnosis? Will she stay in touch to make sure that you recover as expected? Can you trust her?
These questions suggest that physician dissatisfaction and physician well-being may be issues worthy of attention. If physician dissatisfaction, for example, affects the quality of care, and if it is widespread, then physician dissatisfaction is a public health issue (Kravitz, 2012). In this paper we present a simple model of hypothesized relationships between physician dissatisfaction, physician well-being, and the quality of care for patients. We briefly review the evidence on the effects of physician dissatisfaction and a lack of physician well-being on quality. We suggest areas where research is lacking and types of research that might address these gaps.
Model of the effects of physician dissatisfaction
By “physician dissatisfaction”, we mean lack of satisfaction related directly to the physician’s work, as reported by the physician. By physician well-being we mean, at a minimum, the absence of burnout, depression, poor self-care, and substance abuse. Research suggests a negative correlation between physician dissatisfaction and well-being, though not all dissatisfied physicians report being burnt out, and not all physicians who report being burned out report being dissatisfied (Keeton, Fenner, Johnson, & Hayward, 2007; Williams, Manwell, Konrad, & Linzer, 2007). Figure 1 presents a simple model of physician well-being and physician dissatisfaction and their possible effects; we discuss research evidence relevant to the components of this model in the “Evidence” section of this paper, below.
Figure 1 assumes that, though physician well-being and physician satisfaction are not identical, the same factors affect both, and that both physician well-being and physician satisfaction may impact physician behavior and therefore the quality of medical care. Multiple factors may affect physician well-being and satisfaction—notably the physician’s income and the conditions in which he or she works—for example work hours, the pace of work, the culture of the organization in which the physician works, the incentives the organization provides to the physician, and administrative or other obstacles that make work more difficult and/or that interfere with the physician’s ability to provide what he or she considers to be high quality care. In addition, if patient outcomes or patients’ experience of care are not as favorable as the physician believes appropriate, this may lead to physician dissatisfaction.
Figure 1 suggests that dissatisfied physicians may be more likely to develop stress, burnout, depression, poor self-care, and/or substance abuse, and that physicians who are stressed, burned-out, depressed, etc. will be more likely to report being dissatisfied with their work. Physician dissatisfaction and physician well-being, in turn, may have an impact on physician behavior: They may diminish the cognitive capacity that the physician applies to her work, the concentration that she is able to bring to bear on difficult problems, the effort that she makes for patients, and the empathy that she is able to feel for her patients. More broadly, and perhaps even more importantly, the physician’s professionalism may be reduced—a topic to which we will return in a moment.
If cognitive capacity, concentration, effort, empathy, and professionalism are reduced, there may be negative impacts on patients: The physician may be more likely to make incorrect diagnoses, to make other medical errors, to write inappropriate prescriptions and to make unnecessary referrals for specialist care and for expensive diagnostic tests, and to perform particularly poorly in areas of medical care that are difficult for patients, peers, or outside entities that measure physician performance to observe. Confronted with a physician who doesn’t give them much time, empathy, or information, patients may be less satisfied with their care and be less likely to adhere to important advice from the physician. Figure 1 suggests a possible deleterious feedback cycle in which physician dissatisfaction and/or low physician well-being lead to lower patient satisfaction and worse outcomes for patients, which in turn increase physician dissatisfaction and/or lower physician well-being.
Related, quite similar models have been published (Firth-Cozens, 2001; Wallace, Lemaire, & Ghali, 2009; Williams & Skinner, 2003), though they do not explicitly distinguish between physician dissatisfaction and physician well-being.
Physician dissatisfaction and lack of physician well-being may also affect patients indirectly. For example, dissatisfied or burnt-out physicians may be more likely to change jobs frequently or to leave medicine altogether. The costs of physician turnover are high for both the physician and the organization that employed her. Higher costs may be passed on to the organizations that pay for medical care, and ultimately to patients. If physicians leave medical practice, they exacerbate the problem, at least in the U.S., of shortages of physicians in some specialties (especially primary care—and primary care physicians tend to be among the most dissatisfied) and geographic areas.
Physician dissatisfaction, physician well-being, and physician professionalism
Physician professionalism has many facets (Medical Professionalism Project, 2002), but for purposes of this article we will focus on two: first, keeping one’s knowledge and skills up to date; second, putting the patient’s needs first. Proponents of physician professionalism often discuss it as if it were a metaphysical essence—a vital inner capacity possessed by almost all physicians (Barondess, 2003). Skeptics, at the extreme, see physician professionalism as a self-serving myth—a shield used by physicians to maximize their autonomy and incomes (Larson, 1977). But it is probably more accurate to understand physician professionalism not as a metaphysical essence, nor as a self-serving myth, but as a vital but variable reality—something that is vital for the well-being of patients but varies depending on the individual physician and the environment in which the physician works.
As the Nobel Prize winning economist Kenneth Arrow pointed out long ago, physician professionalism is important because of the inevitable information asymmetry between patients and physicians (Arrow, 1963). Patients generally cannot know as much as physicians, and neither patients nor any outside entity (such as a government agency or a health insurance company) can observe or measure all—or even very many—of the important decisions physicians make and the important things they do (or don’t do) for patients. Therefore, even in health care systems that emphasize “pay-for performance,” public reporting of physician performance, and/or “value based payment,” physician professionalism will remain very important if patients are to receive truly high quality care (Casalino, 1999).
Put another way, physician professionalism is important because highly professional physicians will try hard to do the right thing even when they are not being measured, and many critical areas of medical care—for example diagnosis—are not currently measured and may never be amenable to accurate measurement (Berenson & Kaye, 2013; Casalino, Alexander, Jin, & Konetzka, 2007). But professionalism is likely to vary across physicians (based, for example, on differences in physicians’ personalities and in the training they have had) and even within the same physician over time (based, for example, on the organization in which the physician works and the incentives that the physician faces).
It seems likely that physicians who are dissatisfied, burned-out, and/or depressed will act less professionally. If this is the case, the impact on patient care is likely to be large. Critically, much of the impact may be difficult to measure, because professionalism is particularly important for areas of patient care that are difficult (or, practically speaking, impossible) to measure (Berenson & Kaye, 2013).
Evidence of the consequences of physician dissatisfaction and low physician well-being
This article is not intended to be a comprehensive review of the literature but rather a presentation of key concepts and key findings from the literature and suggestions for research to fill important gaps in the literature. We focused our search of the literature on the consequences of physician dissatisfaction, but we also report evidence on the impact of poor physician well-being. Specifically, we searched PubMed, Google Scholar, and Google for the phrases “physician satisfaction” and “physician dissatisfaction,” with emphasis on the past 25 years. To our knowledge, there have been two narrative reviews in English of research on the consequences of physician dissatisfaction and low physician well-being, with the most recent published in 2009 (Wallace et al., 2009; Williams & Skinner, 2003). We critically and selectively present evidence from these reviews, as well evidence that has appeared since they were published.
Physician well-being
Many physicians work long hours and must deal with various kinds of stressors. Suicide rates tend to be higher among physicians than among the general population (Hem et al., 2005). There is ample evidence that physicians—regardless of the country in which they work—frequently suffer from burnout, depression, and substance abuse problems (Wallace, Lemaire, Ghali, 2009). A recent review cites studies suggesting the frequency of physician reported burnout as ranging from 25-60% (Wallace et al., 2009). A critical assessment of the studies suggests that the true frequency is more likely to be closer to the lower percentage than the higher one, with depression rates somewhat lower than burnout rates. Not surprisingly, dissatisfied physicians are more likely to report being burned out (Williams et al., 2007) and burnout has been shown to be a predictor of physician dissatisfaction (Keeton et al., 2007), though most studies do not evaluate the relationship between dissatisfaction and burnout or depression.
The high frequency of physician burnout contrasts sharply with the high percentage of physicians in the U.S. who reported being “somewhat satisfied” or “very satisfied” with their careers in a large national study (Christopher, Smith, Tivis, & Wilper, 2014) or the fact that physicians scored higher than any other occupational category in overall well-being as measured in a 2012 Gallup Poll (Witters, 2013). This contrast has not been explained and is an important subject for future research. Speculatively, it might be hypothesized that physicians can be satisfied with their careers yet take pride in working very hard and being “burned out”—attitudes that may be imprinted on medical students and resident physicians during their clinical training years.
Physician turn-over and physicians leaving the practice of medicine
There is ample evidence that dissatisfied physicians are more likely to report planning to leave their current practice situation or to leave the practice of medicine altogether (Campbell, Sonnad, Eckhauser, Campbell, & Greenfield, 2001; Sibbald, Bojke, & Gravelle, 2003; Williams et al., 2010; Williams & Skinner, 2003). It is not surprising that dissatisfied physicians would report this, but do they actually leave? A longitudinal study a U.S. national sample of nearly 17,000 physicians, using successive waves of the Community Tracking Study, demonstrated that dissatisfied physicians are in fact more likely to leave medicine or to reduce their work hours (Landon, Reschovsky, Pham, & Blumenthal, 2006). Physicians who reported being very dissatisfied in 1996 were 2.3 times more likely to have left medicine by 1998 and 3.6 times more likely to have reduced their hours practicing medicine. A separate longitudinal study of 507 primary care physicians found that dissatisfied physicians were 2.4 times more likely to leave their current practice (Buchbinder, Wilson, Melick, & Powe, 2001).
Physician professionalism
There is relatively little direct evidence of the effect of dissatisfaction or low physician well-being on physician professionalism. However, as predicted in the model in Figure 1, physicians who report being burned out are more likely to report engaging in unprofessional behaviors and holding less altruistic views about physicians’ responsibility to society (Dyrbye et al., 2010), and physicians who report being stressed report multiple ways in which stress reduces their empathy and cognitive capacity, leading to serious medical errors (Firth-Cozens & Greenhalgh, 1997). In a 2014 study of physicians within a highly esteemed U.S. medical group, one quarter of physicians reported that they depersonalize patients, responding affirmatively to statements such as “I’ve become more callous toward people since I took this job” and “I feel I treat some recipients as if they were impersonal objects” (Goitein, 2014; West et al., 2014).
Patient satisfaction
Research tends to support the hypothesis that patient satisfaction is higher among patients of more satisfied physicians, though the quantity and strength of the research are surprisingly modest. In a 1985 study of patients in 16 academic general internal medicine clinics, patient satisfaction was significantly higher among patients of physicians who reported high levels of satisfaction with their work (Linn et al., 1985).
In a 2005 prospective study of 2,004 patients with pain and/or depression cared for by 261 primary care physicians in private practice in Seattle, patients reported significantly higher trust and confidence in physicians who had high job satisfaction, and depressed patients gave higher ratings to the care provided by high satisfaction physicians, but neither pain nor depression patients reported significantly better communication with their physicians (Grembowski et al., 2005).
In a 2008 study of patients who had been hospitalized for a variety of reasons, among 178 matched physician-patient pairs, patients of physicians who scored high on the depersonalization dimension of the Maslach Burnout Inventory were less satisfied with their physician and reported a longer post-discharge recovery time (Halbesleben & Rathert, 2008).
Patient adherence to physician recommendations
There is surprisingly little direct evidence on the relationship of physician satisfaction to patient adherence with physician recommendations. In a 1993 two year prospective study of 20,000 chronically ill patients of 186 physicians, patients were more likely to follow the recommendations of physicians who reported relatively high levels of global satisfaction with their practice of medicine (DiMatteo et al., 1993). A 1985 study found higher continuity of care and lower patient no-show rates in internal medicine practices when both physicians and patients reported higher satisfaction (Linn et al., 1985); more highly satisfied physicians also had patients with better adherence in a two year study of 186 physicians (DiMatteo et al., 1993).
Prescribing medications and referring patients to specialists
Dissatisfied physicians may not be inclined to devote too much time or cognitive effort to caring for their patients. If this is true, then it is easier to write a prescription and send the patient on her way than to spend time evaluating a problem thoroughly and communicating with the patient. Similarly, if a patient’s problem is at all difficult, it is quicker simply to refer the patient to another physician, or for an imaging study (except in environments where referrals are rationed and making a referral may require some time from the physician). There is a good deal of evidence that dissatisfied physicians write more prescriptions, and some evidence that they make more referrals. In a 1980 cross-sectional study of 124 general practitioners in England and Wales, physicians with low job satisfaction were significantly more likely to prescribe medications that are prone to cause adverse reactions (such as monoamine oxidase inhibitors, or major tranquilizers for elderly patients) and/or were deemed inappropriate (Melville, 1980).
In a 1985 cross-sectional study of 42 general practitioners in the Netherlands, dissatisfied physicians prescribed more medications (Grol et al., 1985). However, they made fewer referrals to specialists. It is not clear whether, in the context in which these physicians were working, referrals were an activity that required little effort from the physician (in which case one might expect dissatisfied physicians to make more referrals) or significant effort from physicians (in which case dissatisfied physicians might make fewer referrals).
In a 2003 cross-sectional study of 220 primary care physicians performed in Barcelona in 2000, physicians classified as burned out, using the Maslach Burnout Inventory, generated significantly higher pharmaceutical costs of prescribing (Cebria, Sobreques, Rodriguez, & Segura, 2003).
In a 2013 cross-sectional study of 135 primary care physicians in one Health Maintenance Organization district in Israel, burned out physicians referred significantly more patients to specialists and for diagnostic imaging tests. Physicians with a higher workload also referred more patients (holding the extent of burnout constant). Fifty-six percent of physicians in this study, which used the Maslach Burnout Inventory, were classified as burned out (Kushnir et al., 2014).
Quality of care
Direct evidence of the relationship between physician satisfaction and the quality of care is relatively scarce and shows mixed results. The difficulty of measuring the quality of care, particularly with small sample sizes, may contribute to these results.
Dissatisfied physicians generally report dissatisfaction with the quality of care they feel able to provide, and vice-versa (Friedberg et al., 2013; Tyssen, Palmer, Solberg, Voltmer, & Frank, 2013). A cross-sectional analysis of 1996 data from the large national Community Tracking Study physician survey found that primary care physicians who reported dissatisfaction with their medical career were significantly more likely to report that in their situation it was more difficult to provide high quality care or to have sufficient communication with specialists (DeVoe, Fryer Jr, Hargraves, Phillips, & Green, 2002). It is not surprising that physicians who are dissatisfied with their work also report being dissatisfied with specific aspects of their work (e.g. the ability to provide high quality care), so the direction of causality is not clear.
Physicians report that fatigue and overwork lead them to treat patients irritably and lead to serious mistakes (Firth-Cozens & Greenhalgh, 1997). In a large, 2010 cross-sectional survey of 8,000 U.S. surgeons, 9% reported making a major medical error in the previous three months (Shanafelt et al., 2010). Physicians who were classified as burned out, using the Maslach Burnout Inventory, or as depressed, were significantly more likely to report making a major medical error. It was not possible to judge whether burnout or depression makes medical errors more likely, or whether making a major medical error leads to burnout or depression, or whether the causality operates in both directions. Bidirectional causality is supported by a 2006 prospective longitudinal cohort study of 184 internal medicine residents that found that committing a self-perceived medical error was associated with a large, significantly increased frequency of subsequent burnout or depression, and that increased burnout was associated with a significantly increased risk of committing a subsequent self-perceived medical error (West, Tan, Habermann, Sloan, & Shanafelt, 2009).
In a 2003 small prospective cohort study of pediatric residents in two children’s hospitals, 20% (24) of the residents met the criteria for depression and 74% (90) of the residents met the criteria for burnout, using the Maslach Burnout Inventory (Fahrenkopf et al., 2008). Depressed residents made significantly more medication errors – more than six times as many errors as residents who were not depressed. There was no difference in error rates between the burned out residents and those who were not burned out.
In a 2005 prospective study of 2,004 patients with pain and/or depression, cared for by 261 primary care physicians in private practice in Seattle, the health status, at 6 month follow-up, of patients who had highly satisfied physicians, did not differ significantly from patients with less satisfied physicians (Grembowski et al., 2005).
A 2008 cross-sectional study of 53 physicians working in 13 hospitals in Japan linked physician survey data to data abstracted from outpatient charts on care of patients with hypertension, diabetes, and asthma (Utsugi-Ozaki, Bito, Matsumura, Hayashino, & Fukuhara, 2009). There was no association between physician satisfaction and the quality of care provided.
In an important 2009 cross-sectional study of 422 primary care physicians and 1,795 chronically ill patients in 119 clinics in New York City and the Midwest, 27% of the physicians reported burnout (Linzer et al., 2009). Burnout was not associated with the quality of care—measured by chart audits of such things as hemoglobin A1c control for patients with diabetes.
Discussion and suggestions for further research
Anecdotal reports suggest an increase in physician burnout in the U.S., yet studies of physician satisfaction continue to show overall rates of U.S. physician satisfaction of about 80% (Christopher, Smith, Tivis, & Wilper, 2014; Friedberg et al., 2013). The most recent nationally representative survey of U.S. physician satisfaction was completed in 2006 (Christopher et al., 2014)—well before health care reform and the very large increase in electronic health records (EHR) that resulted from the financial incentives for EHR implementation provided by the federal Meaningful Use program (Blumenthal, 2011). There are some indications that during recent years EHRs have been a major factor in U.S. physician dissatisfaction (Friedberg et al., 2013). It is possible that physician satisfaction in the U.S. has declined during the past eight years, though the 2012 Gallup study indicates that at that time physicians were still the most satisfied occupation in the U.S. (Witters, 2013).
Studies of the prevalence of physician burnout provide very high prevalence percentages, suggesting that some physicians are reporting symptoms of burnout yet are satisfied with their career. The 2013 RAND study, in which 81% of a (non-nationally representative) sample of physicians stated that they are satisfied with their career, yet 27% reported feeling burned out, showed that this in fact does occur (Friedberg et al., 2013). It would be useful to have studies that provide information on the relationship between satisfaction and burnout.
Overall, the available evidence supports the hypotheses suggested by the model in Figure 1. There is strong evidence, including two longitudinal studies, that dissatisfied physicians are more likely to work less, to leave medicine, and/or to state that they would not advise young people to become physicians. Though the number of physicians leaving medicine does not appear to be large, it is not a good thing for physician supply to be reduced at a time when health care reform is increasing demand by increasing the number of insured patients in the U.S. and when the U.S. has a worsening shortage of primary care physicians.
In addition, though the evidence is not overwhelming, and though high quality studies are few, it does appear that physician dissatisfaction and burnout have a negative impact on patients. There is surprisingly little evidence about the relationship between physician satisfaction and patient satisfaction, but the available evidence, including one large prospective study, does suggest that satisfied physicians are more likely to have satisfied patients. There is very little evidence about the relationship between physician satisfaction and patient adherence to physicians’ recommendations, but the one large prospective study that exists supports this relationship. There is a good deal of evidence, albeit all from cross-sectional studies, that dissatisfied physicians are more likely to write prescriptions, including inappropriate prescriptions, and to refer patients to specialists and for imaging studies (though the appropriateness of these referrals has not been studied). There is relatively little evidence of the relationship between physician satisfaction and measures of the quality of care; the evidence to date, including three prospective studies, does not show a strong relationship. This may be because physician satisfaction is not related to quality, though it is more likely, give the other evidence just cited, that the relationship has not been demonstrated because of small sample sizes and difficulties with adequately measuring quality.
If dissatisfied physicians act less professionally, this would be expected to have a pervasive effect on quality—especially on areas of quality that are not usually measured. Very little evidence concerning the relationship between physician dissatisfaction and physician professionalism exists, though the evidence that does exist suggests that there may be a strong relationship. Research in this area is hindered by the lack of accepted measures of professionalism in practicing physicians.
Most studies of the effects of physician satisfaction have been flawed by one or more of the following: low physician response rates with possible accompanying selection bias, small samples, a cross-sectional design that makes it difficult to assess the direction of causality (if any), and the problem, inherent in observational research, that confounding factors may affect both physician satisfaction and the dependent variable (e.g., the quality of care provided). For example, certain physicians might have personalities that make them both more likely to report being dissatisfied and more likely to provider poor quality care. In this case, one might want to avoid dissatisfied physicians, but the dissatisfaction would not be causing the poor quality.
Physician dissatisfaction might be a warning sign that the physician and/or the organization within the physician works are providing quality of care that is less than desirable (Friedberg et al., 2013). This will be true to the extent that dissatisfied physicians provide worse care and/or to the extent that physicians are dissatisfied because they believe that the conditions under which they work are obstacles to providing high quality care (see Figure 1, page 10). However, it is possible that not all causes of physician dissatisfaction have the same implications for quality. For example, a physician who is dissatisfied because his or her income is too low may provide lower quality care, but their dissatisfaction is not in itself an indication that the conditions under which the physician works are obstacles to quality. It would be very useful for researchers to investigate the extent to which physician dissatisfaction is an indicator that quality may be poor, and to investigate whether different causes of dissatisfaction vary in their implications for quality.
It will never be possible to conduct randomized trials of the relationship between physician satisfaction and physician professionalism, or of the relationship between physician satisfaction and the quality of patient care. However, it would be possible to conduct studies that are prospective, are larger, obtain high response rates from physicians, and have a stronger analytic design. Ideally, this design might include difference in differences analyses that compare patient satisfaction, patient adherence, and the quality of care for patients of physicians who become dissatisfied to those who remain satisfied, and vice versa. These studies would not be inexpensive, but the topic is extremely important. Large sums of money are being invested in comparative effectiveness research that supports evidence-based medical decisions, but this research will be useless if dissatisfied physicians ignore it.
References
- Arrow, K. (1963). Uncertainty and the Welfare Economics of Medical Care. The American Economic Review, 53(5), 941-969.
- Barondess, J. A. (2003). Medicine and professionalism. Archives Internal Medicine, 163(2), 145-149. https://doi.org/10.1001/archinte.163.2.145
- Berenson, R. A., & Kaye, D. R. (2013). Grading a physician's value—the misapplication of performance measurement. New England Journal of Medicine, 369(22), 2079-2081. https://doi.org/10.1056/NEJMp1312287
- Blumenthal, D. (2011). Wiring the Health System: Origins and Provisions of a New Federal Program. New England Journal of Medicine, 365(24), 2323-2329. https://doi.org/10.1056/NEJMsr1110507
- Buchbinder, S. B., Wilson, M., Melick, C. F., & Powe, N. R. (2001). Primary care physician job satisfaction and turnover. The American Journal of Managed Care, 7(7), 701-713.
- Campbell, D. A., Sonnad, S. S., Eckhauser, F. E., Campbell, K. K., & Greenfield, L. J. (2001). Burnout among American surgeons. Surgery, 130(4), 696-702. https://doi.org/10.1067/msy.2001.116676
- Casalino, L. P. (1999). The unintended consequences of measuring quality on the quality of medical care. New England Journal of Medicine, 341(15), 1147-1150. https://doi.org/10.1056/NEJM199910073411511
- Casalino, L. P., Alexander, G. C., Jin, L., & Konetzka, R. T. (2007). General internists’ views on pay-for-performance and public reporting of quality scores: a national survey. Health Affairs, 26(2), 492-499. https://doi.org/10.1377/hlthaff.26.2.492
- Cebria, J., Sobreques, J., Rodriguez, C., & Segura, J. (2003). Influence of burnout on pharmaceutical expediture among primary care physicians. Gaceta Sanitaria, 17(6), 483-489.
- Christopher, A. S., Smith, C. S., Tivis, R., & Wilper, A. P. (2014). Trends in United States physician work hours and career satisfaction. The American Journal of Medicine, 127(7), 674-680. https://doi.org/10.1016/j.amjmed.2014.03.033
- DeVoe, J., Fryer, G. E., Hargraves, J. L., Phillips, R. L., & Green, L. A. (2002). Does career dissatisfaction affect the ability of family physicians to deliver high-quality patient care? The Journal of Family Practice, 51(3), 223-228.
- DiMatteo, M. R., Sherbourne, C. D., Hays, R. D., Ordway, L., Kravitz, R. L., McGlynn, E. A., Sherrie, Kaplan, & Rogers, W. H. (1993). Physicians' characteristics influence patients' adherence to medical treatment: results from the Medical Outcomes Study. Health Psychology, 12(2), 93-102. https://doi.org/10.1037/0278-6133.12.2.93
- Dyrbye, L. N., Massie, F. S., Jr., Jr., Eacker, A., Harper, W., Power, D., Durning, S. J., Thomas, M. R., Moutier, C., Satele, D., Sloan, J., & Shanafelt, T. D. (2010). Relationship between burnout and professional conduct and attitudes among US medical students. Jama, 304(11), 1173-1180. https://doi.org/10.1001/jama.2010.1318
- Fahrenkopf, A. M., Sectish, T. C., Barger, L. K., Sharek, P. J., Lewin, D., Chiang, V. W., Edwards, S., Wiedermann, B. L., & Landrigan, C. P. (2008). Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ, 336(7642), 488-491. https://doi.org/10.1136/bmj.39469.763218.BE
- Firth-Cozens, J. (2001). Interventions to improve physicians' well-being and patient care. Social Science & Medicine, 52(2), 215-222. https://doi.org/10.1016/S0277-9536(00)00221-5
- Firth-Cozens, J., & Greenhalgh, J. (1997). Doctors' perceptions of the links between stress and lowered clinical care. Social Science & Medicine, 44(7), 1017-1022. https://doi.org/10.1016/S0277-9536(96)00227-4
- Friedberg, M. W., Chen, P. G., Van, K. R., Aunon, F. M., Pham, C., Caloyeras, J. P., & Tutty, M. (2013). Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Boston, MA: The RAND Corporation.
- Goitein, L. (2014). Physician well-being: Addressing downstream effects, but looking upstream. JAMA Internal Medicine, 174(4), 533-534. https://doi.org/10.1001/jamainternmed.2013.13253
- Grembowski, D., Paschane, D., Diehr, P., Katon, W., Martin, D., & Patrick, D. L. (2005). Managed care, physician job satisfaction, and the quality of primary care. Journal of General Internal Medicine, 20(3), 271-277. https://doi.org/10.1111/j.1525-1497.2005.32127.x
- Grol, R., Mokkink, H., Smits, A., van, J., Beek, M., Mesker, P., & Mesker-Niesten, J. (1985). Work satisfaction of general practitioners and the quality of patient care. The Journal of Family Practice, 2(3), 128-135. https://doi.org/10.1093/fampra/2.3.128
- Halbesleben, J. R., & Rathert, C. (2008). Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Management Review, 33(1), 29-39. https://doi.org/10.1097/01.HMR.0000304493.87898.72
- Hem, E., Haldorsen, T., Aasland, O. G., Tyssen, R., Vaglum, P., & Ekeberg, Ø. (2005). Suicide among physicians. The. American Journal of Psychiatry, 162(11), 2199-2200. https://doi.org/10.1176/appi.ajp.162.11.2199-a
- Keeton, K., Fenner, D. E., Johnson, T. R., & Hayward, R. A. (2007). Predictors of physician career satisfaction, work-life balance, and burnout. Obstetrics Gynecology, 109(4), 949-955. https://doi.org/10.1097/01.AOG.0000258299.45979.37
- Kravitz, R. L. (2012). Physician job satisfaction as a public health issue. Israel Journal of Health Policy Research, 1(1), 51. https://doi.org/10.1186/2045-4015-1-51
- Kushnir, T., Greenberg, D., Madjar, N., Hadari, I., Yermiahu, Y., & Bachner, Y. G. (2014). Is burnout associated with referral rates among primary care physicians in community clinics? The Journal of Family Practice, 31(1), 44-50. https://doi.org/10.1093/fampra/cmt060
- Landon, B. E., Reschovsky, J. D., Pham, H. H., & Blumenthal, D. (2006). Leaving medicine: the consequences of physician dissatisfaction. Medical Care, 44(3), 234-242. https://doi.org/10.1097/01.mlr.0000199848.17133.9b
- Larson, M. (1977). The Rise of Professionalism: A Sociological Analysis. Berkeley, CA: University of California Press.
- Linn, L. S., Brook, R. H., Clark, V. A., Davies, A. R., Fink, A., & Kosecoff, J. (1985). Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Medical Care, 23(10), 1171-1178. https://doi.org/10.1097/00005650-198510000-00006
- Linzer, M., Manwell, L. B., Williams, E. S., Bobula, J. A., Brown, R. L., Varkey, A. B., Man, B., McMurray, J. E., Maguire, A., Horner-Ibler, B., & Schwartz, M. D. (2009). Working conditions in primary care: physician reactions and care quality. Annals of internal medicine, 151(1), 28-36. https://doi.org/10.7326/0003-4819-151-1-200907070-00006
- Medical Professionalism Project. (2002). Medical Professionalism in the New Millennium: A Physician Charter. Annals of Internal Medicine, 136(3), 243-246. https://doi.org/10.7326/0003-4819-136-3-200202050-00012
- Melville, A. (1980). Job satisfaction in general practice implications for prescribe ing. Social Science & Medicine. Part A: Medical Psychology & Medical Sociology, 14(6), 495-499. https://doi.org/10.1016/S0271-7123%2880%2980055-1
- Shanafelt, T. D., Balch, C. M., Bechamps, G., Russell, T., Dyrbye, L., Satele, D., Collicott, P., Novotny, P .J., Sloan, J., & Freischlag, J. (2010). Burnout and medical errors among American surgeons. Annals of Surgery, 251(6), 995-1000. https://doi.org/10.1097/SLA.0b013e3181bfdab3
- Sibbald, B., Bojke, C., & Gravelle, H. (2003). National survey of job satisfaction and retirement intentions among general practitioners in England. BMJ, 326(7379). https://doi.org/10.1136/bmj.326.7379.22
- Tyssen, R., Palmer, K. S., Solberg, I. B., Voltmer, E., & Frank, E. (2013). Physicians' perceptions of quality of care, professional autonomy, and job satisfaction in Canada, Norway, and the United States. BMC health services research, 13, 516. https://doi.org/10.1186/1472-6963-13-516
- Utsugi-Ozaki, M., Bito, S., Matsumura, S., Hayashino, Y., & Fukuhara, S. (2009). Physician job satisfaction and quality of care among hospital employed physicians in Japan. Journal of General Internal Medicine, 24(3), 387-392. https://doi.org/10.1007/s11606-008-0886-4
- Wallace, J. E., Lemaire, J. B., & Ghali, W. A. (2009). Physician wellness: a missing quality indicator. Lancet, 374(9702), 1714-1721. https://doi.org/10.1016/S0140-6736%2809%2961424-0
- West, C. P., Dyrbye, L. N., Rabatin, J. T., Call, T. G., Davidson, J. H., Multari, A., Romanski, S. A., Henriksen Hellyer, J. M., Sloan, J. A., & Shanafelt, T. D. (2014). Intervention to Promote Physician Well-being, Job Satisfaction, and Professionalism: A Randomized Clinical Trial. JAMA Internal Medicine, 174(4), 527-533. https://doi.org/10.1001/jamainternmed.2013.14387
- West, C. P., Tan, A. D., Habermann, T. M., Sloan, J. A., & Shanafelt, T. D. (2009). Association of resident fatigue and distress with perceived medical errors. Jama, 302(12), 1294-1300. https://doi.org/10.1001/jama.2009.1389
- Williams, E. S., Konrad, T. R., Scheckler, W. E., Pathman, D. E., Linzer, M., McMurray, J. E., & … Schwartz, M. (2010). Understanding physicians' intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical health. 2001. Health Care Management Review, 35(2), 105-115. https://doi.org/10.1097/01.HMR.0000304509.58297.6f
- Williams, E. S., Manwell, L. B., Konrad, T. R., & Linzer, M. (2007). The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Management Review, 32(3), 203-212. https://doi.org/10.1097/01.HMR.0000281626.28363.59
- Williams, E. S., & Skinner, A. C. (2003). Outcomes of physician job satisfaction: a narrative review, implications, and directions for future research. Health Care Managment Review, 28(2), 119-139. https://doi.org/10.1097/00004010200304000-00004
- Witters, Dan. (2013, March 13). U.S. Doctors Lead in Wellbeing, Transportation Workers Lag. Retrieved from http://www.gallup.com/poll/161324/physicians-lead-wellbeing-transportation-workers-lag.aspx