Peter Angerer and Matthias Weigl
Physicians' psychosocial work conditions and quality of care: A literature review
Abstract: Background: Physician jobs are associated with adverse psychosocial work conditions. We summarize research on the relationship of physicians' psychosocial work conditions and quality of care. Method: A systematic literature search was conducted in MEDLINE and PsycINFO. All studies were classified into three categories of care quality outcomes: Associations between physicians' psychosocial work conditions and (1) the physician-patient-relationship, or (2) the care process and outcomes, or (3) medical errors were examined. Results: 12 publications met the inclusion criteria. Most studies relied on observational cross-sectional and controlled intervention designs. All studies provide at least partial support for physicians’ psychosocial work conditions being related to quality of care. Conclusions: This review found preliminary evidence that detrimental physicians’ psychosocial work conditions adversely influence patient care quality. Future research needs to apply strong designs to disentangle the indirect and direct effects of adverse psychosocial work conditions on physicians as well as on quality of care.
Keywords: psychosocial work conditions; physicians; quality of care; physician-patient-relationship; hospital; errors; review; work stress; clinicians
Adverse psychosocial work conditions as conceptualized in the work stress models of job-demand-control-support, effort-reward imbalance, and organizational justice have been shown to affect well-being and mental health of workers (Stansfeld & Candy, 2006). This relationship is also true in health care professionals with particular focus on physicians (Buddeberg-Fischer, Klaghofer, Stamm, Siegrist, & Buddeberg, 2008; Firth-Cozens, 2003; Tyssen & Vaglum, 2002; Weigl, Hornung, Petru, Glaser, & Angerer, 2012). Clearly, physicians have a great impact on the quality of care in various ways such as through their medical skills, communication with patients, decisions in diagnostics and treatment, as well as coordination and communication with other professions involved in care delivery. Stressed or mentally ill health care personnel is a risk factor for the quality of care and patient safety. Research showed that physicians with burnout symptoms (as an early reaction to work stress) or depression perform worse and make more mistakes (Fahrenkopf et al., 2008; Lee, Seo, Hladkyj, Lovell, & Schwartzmann, 2013; Shanafelt, Bradley, Wipf, & Back, 2002; West et al., 2006).
In this research, we argue that adverse psychosocial work conditions may also influence the quality of care directly. We sought for studies that investigated the associations between physicians’ psychosocial work conditions and outcomes related to quality of patient care. We focused on three major outcomes relevant for care quality: (1) physicians' and/or patients' perceptions of quality of care, (2) success of treatment or the absence of complications, and (3) prevalence of medical errors.
Previous evidence on physicians’ psychosocial work conditions and care quality
In regard to health care professionals, effects of work conditions on quality of care outcomes were addressed previously in two reviews (Hickam et al., 2003; Kapinos, Fitzgerald, Greer, Rutks, & Wilt, 2012). Hickam and colleagues (2003) extensively reviewed the scientific literature on the impact of health care work conditions on patient safety. In their well-conducted review among various health-care professionals they found that several facets of adverse work conditions in health care affect patient safety. However, they concluded that the evidence was drawn from merely a few studies and was insufficient to draw clear conclusions. Adverse psychosocial work conditions of physicians as defined in the present study were not in the focus of Hickam et al.’s review, and there was only one study that adequately covered this matter (Jones et al., 1988). Furthermore, the outcome of interest was limited to patient safety.
Kapinos and colleagues (2012) focused on primary care providers and reviewed evidence on the role of work conditions in influencing patient outcomes and healthcare quality. Overall, they found that reduced workload and shorter work hours, frequent provider training, and computerized systems result in higher quality of patient care. However, no effect was observed for patient satisfaction (Kapinos et al., 2012). Furthermore, they conclude that the overall study base is limited. Only one of the reviewed studies (Linzer et al., 2009) dealt with the research question of the present study.
Both reviews provided important insights into the nature of adverse work conditions and their effect on quality of care. However, they did not specifically focus on physicians and only addressed a limited range of psychosocial risk factors in the work environment of healthcare professionals. We thus set out to identify and summarize evidence from the current literature base specifically on the effects of physicians’ psychosocial work conditions as conceptualized below on effects in care quality.
Conceptualization of psychosocial work conditions
Occupational stress models postulate that psychosocial work conditions, belonging to categories of work tasks, work organization, social relationships at work, and environmental conditions, may have an impact on employees. Many models distinguish between “job demands,” which encompass work conditions that require mental or physical energy to cope with (e.g. time pressure, social conflicts). Furthermore, there are “job resources” that support employees in accomplishing their work goals (e.g., autonomy, social support, esteem). There are several well-established conceptualizations of adverse psychosocial work conditions, often synonymously termed "work stress.” In our review, we focus on three prominent models:
The most popular model is the job-demand-control (JDC) model (Karasek, 1979). It postulates that high job demands (e.g., high work load, time pressure) adversely affect well-being and health, particularly when employees have low job control (e.g., limited decisions on when and how to do their work). Various epidemiological studies demonstrate that the combination of high job demands and low job control increases the risk of mental disorders (Stansfeld & Candy, 2006). Subsequent research added the specific role of social support by supervisors or colleagues to the initial model, which can directly reduce work stress or buffer the effect of job demands and limited job control on health and well-being (Johnson & Hall, 1988).
A second model in occupational health psychology is the Effort-Reward Imbalance (ERI) Model by Siegrist (1996). It draws on the assumption that fair exchange is a fundamental feature of good workplaces. In accordance to efforts invested (e.g., working under time pressure), employees expect adequate rewards (e.g., salary, esteem, career opportunities, and job security) so that a perceived balance between efforts and rewards is achieved and maintained. Broad empirical evidence demonstrates that a mismatch of high efforts and low rewards increases the risk of physical and mental ill-health (e.g., Stansfeld & Candy, 2006).
Organizational justice adds the concept of procedural and interpersonal fairness (Greenberg, 1990) to the above mentioned work stress models. Procedural justice describes a state where employees are informed about important organizational matters and are involved in important decisions. Conversely, relational justice refers to the fair and respectful treatment of employees by their supervisors. Previous studies confirm that organizational justice is related to psychiatric disorders (Elovainio, Heponiemi, Sinervo, & Magnavita, 2010; Ndjaboue, Brisson, & Vezina, 2012).
Pathways between physicians’ work conditions and quality of care
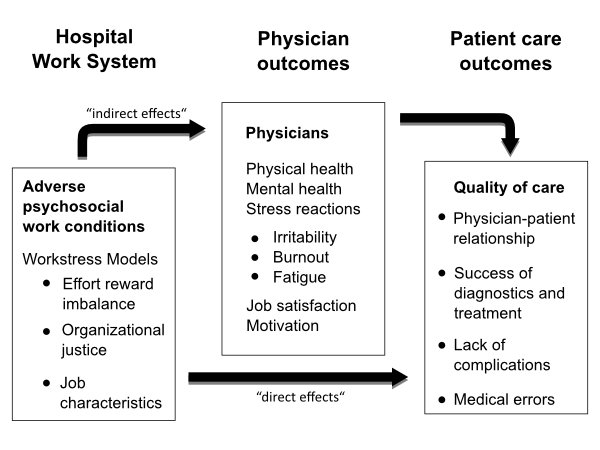
In our review, we propose that physicians’ psychosocial work conditions directly as well as indirectly affect care quality. In regard to indirect pathways, we argue that adverse psychosocial work conditions put physicians under an exceeding psychological burden, resulting in work stress and thus influencing professional behavior. This pathway could be explained by limited physicians’ performance capacity, which is due to work conditions that cause work stress; for example frequent distractions can increase physicians’ mental workload, which consequently compromises professional performance (Weigl, Müller, Vincent, Angerer, & Sevdalis, 2012). Further detrimental effects of work stress could be attentional narrowing, distraction, and loss of working memory. Eventually, these altered behavioral processes adversely affect professional judgments, decision making, motivation or satisfaction and consequently increase the likelihood of medical malpractice and poor quality of work (Jones et al., 1988).
Concerning direct effects of physicians’ work conditions to quality of care, we draw from a system approach to quality and safety in health care (Dekker, 2011; Lawton et al., 2012; Vincent, Moorthy, Sarker, Chang, & Darzi, 2004). System approaches to health care differentiate between immediate individual threats to high-quality performance, such as fatigue and strain, and systemic threats arising from poorly designed care environments, for example unfavorable staffing numbers or high patient census (Hoff, Jameson, Hannan, & Flink, 2004). According to this approach, a high-risk work environment has inherent weaknesses that manifest themselves in work stressors and promote errors and low-quality performance (Carayon et al., 2006; Lawton et al., 2012; Vincent et al., 2004). Both proposed pathways are illustrated in Figure 1:
Research question
This review’s aim was to summarize and discuss the current literature on the associations between physicians’ psychosocial work conditions as conceptualized in the section above and quality of care. Outcomes of interest in physicians’ quality of care were defined by means of the following indicators that reflect the categories of patient centeredness, effectiveness, and safety:
(1) Physicians' and patients' perception of quality of care: This outcome refers to quality of care perceived by physicians and patients. It relates to patient centeredness of clinical activities and the physician-patient relationship as well as to physician empathy, accessibility, reliability and exchange of information.
(2) Success of treatment and absence of complications: This outcome includes effectiveness, which is conceptualized as success of treatment, i.e., various indications of treatment success, clinical quality, or lack of treatment complications.
(3) Prevalence of medical errors: This outcome refers to safety of care, which was conceptualized as medical errors, for example medication errors, drug administration or surgical errors, and so on.
Methods
We conducted a literature search on PubMed and PsycINFO to review empirical studies in the scope of the above reported research questions. The following search terms were used: “work stress,” job strain,” “job control,” work control,” “effort reward imbalance,” “injustice,” “support,” “job resources,” “working conditions,” “safety culture,” “work load,” “time pressure,” “interruptions,” “physician work life,” “team,” “supervision,” “leadership,” “fatigue,” “burnout” AND “patient orientation,” “care quality,” “patient care,” “patient safety,” “adverse events,” “prescribing errors,” “medication errors,” “drug administration errors,” “patient outcomes,” “medical errors,” “safety incidents,” “patient harm.” The search included all articles from the start of the data bases until December 2013. Additionally, we searched the reference lists of the two above-mentioned comprehensive reviews (Hickam et al., 2003; Kapinos et al., 2012).
Eligible were original articles in English and German. The following inclusion criteria were applied to eligible articles: (1) physicians are surveyed, (2) assessment of psychosocial work conditions, and (3) measurements of quality of care. Both authors independently reviewed the retrieved articles. Furthermore, eligible were randomized controlled trials, quasi-experimental, longitudinal or cohort studies as well as cross-sectional studies. Ecologic studies, case reports, case series, qualitative and economic evaluations were excluded from analysis. Disagreements between reviewers on the eligibility of retrieved research involved double checks and were resolved by discussion.
The retrieved literature was extracted, summarized and classified according to our three research questions.
Results
The database search identified 814 records, while hand search of retrieved articles identified another seven. Thus 821 records were screened, where of 804 were excluded because they were not within the scope of this review. In the next step, 17 full-text articles were assessed, where of five were excluded as they did not address our target group, that is, physicians. Finally 12 publications of which one reports four studies met the inclusion criteria. The retrieved studies were heterogeneous in regard to design, setting, measurement, medical specialty, and outcome. Thus, meta-analytic calculations and other measures of systematic quantitative aggregation were not appropriate. Instead, we reviewed and aggregated the heterogeneous studies qualitatively. All selected studies are depicted in Table 1-3 in the appendix.
Outcome 1: Physicians’ psychosocial work conditions and physicians’/patients’ perceived care quality.
First, we focused on investigations of physicians’ psychosocial work conditions and quality of care as reported by physicians and patients (see Table 1 in the appendix). There were five studies that measured both physicians’ work conditions and quality of care as well as established a relationship between these concepts. Quality of care was either rated by physicians themselves (Klein, Grosse, Blum, & von dem Knesebeck, 2011) or by their patients (Mache, Vitzthum, Klapp, & Groneberg, 2012; Weigl, Hoffmann, Muller, Barth, & Angerer, 2014; Weigl, Hornung, Angerer, Siegrist, & Glaser, 2013). Three out of five studies were observational with a cross-sectional design, while two studies were experimental with a control-group design. All five research papers involved surgeons, internists, pediatricians, or other specialties from various hospitals. The surveyed work conditions ranged from “moral characteristics” (control of work, support/relationships at work as components of a mixed-measures assessment) (McKinstry et al., 2007), to established work stress models (job strain, effort-reward imbalance). Assessments were either based on self-reports of hospital work conditions (Weigl et al., 2013) or expert-based observations (Weigl et al., 2014).
In spite of the differences, the studies consistently show that better work conditions are related to improved quality of care. Furthermore, both intervention studies indicate that promoting physicians’ work conditions is associated with improved patients’ evaluations of care (Weigl et al., 2014; Weigl et al., 2013).
Outcome 2: Physicians’ psychosocial work conditions and treatment success or absence of complications.
Secondly, we summarized studies on physicians’ psychosocial work conditions and success of treatment or lack of complications in patients (see Table 2 in the appendix). Similarly to outcome 1, only few studies examined this relationship. We identified four studies with relevant outcomes such as hospital acquired infections, hypertension control, and diabetes control.
Associations between physicians’ work conditions and their diabetic patients’ glycemic control have been shown by two large cross-sectional studies investigating outpatient clinics in the US (Linzer et al., 2009) as well as Finnish primary care health centers (Koponen et al., 2013; Virtanen et al., 2012). The studies linked work conditions assessed by entire teams, that is, by physicians, nurses and other health care professionals, with the quality of health care in treated patients. Particular strengths of both studies are the unit-based measurement of treatment success by objective laboratory parameters and objective assessments of infections. Work conditions, for example job control, trust in the organization, leadership values alignment (involving participation in organizational issues, justice, and fairness), procedural justice, and high job stress were associated with inferior quality of care. No consistent association was found for hypertension control (Linzer et al., 2009). Hospital acquired infections were associated with low justice in work distribution, high effort-reward imbalance, low trust and poor collaboration in teams (Virtanen et al., 2009).
Outcome 3: Physicians’ psychosocial work conditions and prevalence of medical errors.
Our third research question referred to studies on physicians’ psychosocial work conditions and the prevalence of medical errors (see Table 3 in the appendix). The four retrieved publications cover seven separate studies (four in Jones et al., 1988; one study each in Linzer et al., 2009; Nielsen, Pedersen, Rasmussen, Pape, & Mikkelsen, 2013; Ross et al., 2013). Five studies apply observations within a cross-sectional design, while two studies describe interventions. Overall, all research papers show that adverse psychosocial work conditions are associated with an increased prevalence of medical errors and malpractice suits. Moreover, two studies show some evidence on the potential of adequate interventions, that is, comprehensive stress management, to reduce errors and malpractice suits in physicians.
Discussion
We set out a comprehensive review of the current knowledge base on associations between physicians’ psychosocial work conditions and quality of care. Our results show that this relationship has been rarely studied yet. However, the studies included in our review clearly affirm the assumption of associations between physicians’ work conditions and quality of care.
Major findings and contributions of this review
Since our review draws on a limited number of studies and a large diversity in settings, designs, participants, and measurements, our conclusions are restricted to a qualitative statement. However, we can infer that there are meaningful and direct associations between physicians’ psychosocial work conditions and quality of care. The identified associations are largely independent from the subjective stress experienced by physicians (i.e., indirect pathway). Furthermore, the reviewed interventions indicate that a change in physicians’ psychosocial work conditions alters quality of care. However, it is neither possible to define the magnitude of effects nor yet justified to estimate overall effect sizes.
These findings corroborate our argument of direct effects between physicians’ psychosocial work conditions and inherent effects on quality of care (see Figure 1). Our argument of a direct pathway between work conditions and quality of care is consistent to system approaches of health care quality and safety, which propose that poorly designed hospital environments pose a systemic threat to patient care quality and safety (Dekker, 2011; Hoff et al., 2004; Lawton et al., 2012; Vincent et al., 2004). Our results provide confirmation for our assumption that adverse psychosocial work conditions are a major indicator for insufficient work and care environments in health care (Carayon et al., 2006). Almost all studies included in this review examined direct associations between physicians’ work conditions and quality of care. Only Linzer et al. (2009) additionally considered physicians' stress reactions and health as an intermediate factor, but did not confirm a mediating effect. Direct associations were investigated in different clinical settings (i.e., in-patient as well as out-patient clinics) and based on various evaluations (as perceived by physicians or patients), while outcomes were operationalized differently (e.g., success of treatment or incidence of errors).
Although the reviewed studies mostly confirm the association between physicians’ psychosocial work conditions and quality of care, not all analyzed work conditions were related to the outcomes in question: Koponen et al. (2013) did not observe a relationship between supervisor support and glycemic control, while Virtanen et al. (2012) did not observe associations between relational justice, effort-reward imbalance, and work-unit team climate and hospital infections as identified in previous research (Virtanen et al., 2009). These findings suggest that not all outcomes concerning quality of care are related to physicians’ work conditions in similar ways. For example, Linzer et al. (2009) revealed associations between work control as well as value alignment and treatment quality of diabetes, but found no effects on patients’ hypertension.
Work overload and multitasking demands limit physicians’ opportunities for direct patient communication. This may explain inferior patient ratings of perceived care as well as wrong decisions due to insufficient time for gathering critical patient information (Mache et al., 2012). In line with this reasoning, work stress can also decrease kindness or empathy of medical staff towards patients (Alarcon & Lyons, 2011; Rousseau & Aube, 2010). However, specific work conditions may act as a buffer or resource in the hypothesized framework (see Figure 1). Adverse work conditions strongly affect physicians’ well-being, but their reactions do not inevitably translate into lower-quality care (Linzer et al., 2009). However, daily hassles and chronic disturbances of well-being may interfere with motivation, satisfaction, and capability of delivering empathetic and highest-standard care in the long term (Koponen et al., 2013).
Comparison of the present review to previous systematic reports
As already described in the introduction, two previous systematic reports addressed the impact of healthcare professionals’ work conditions and quality of care. Our review adds to the current evidence base on this relationship. The first review by Hickam and colleagues (Hickam et al., 2003) investigated effects of work conditions in health care on patient safety. Only Jones et al.’s (1988) study was included in the present review. Furthermore, both systematic reviews are in line with this report’s conclusions that interventions and translational research are warranted in order to modify working conditions with the goal of improving patient safety. Potential fields of application with promising perspectives include: changes in nursing staffing, channeling high-risk technical procedures to high-volume physicians, avoidance of distractions in the workplace, and processes to improve information exchange between hospital and non-hospital settings (Hickam et al., 2003).
Recently published, the second report focused on the effects of work conditions on patient care in primary care settings (Kapinos et al., 2012). It concluded that a feasible workload and shorter work hours, more provider training, and computerized systems are likely to result in higher quality of patient care.
Limitations
Our findings need to be interpreted with caution. Many studies had cross-sectional designs which do not allow conclusions about causality. Thus, the observed associations may be reciprocal, where the experience of a reduced quality of care also leads to a more critical evaluation of work conditions. Although all quantitative studies controlled for a variety of covariates (see Table 1-3 in the appendix), influences of other confounding variables cannot be entirely excluded. Interventional studies with control group design aim at limiting the problem of confounding and allow conclusions about causality (Jones et al., 1988; Weigl et al., 2014; Weigl et al., 2013). However, Jones et al.’s comprehensive study (1988), including 22 intervention and 22 control hospitals, has not been reproduced to date. Two studies by Weigl et al. (Weigl et al., 2014; Weigl et al., 2013) are based on comparatively small physician and patient samples. Thus, our preliminary results indicate that larger intervention studies across different clinical settings are warranted.
All reviewed studies relied on convenience samples with limitations to validity and generalizability. Included studies from different clinical environments provide some evidence for relationships between work conditions and quality of care in different clinical domains. Evaluations of physicians’ work conditions mostly relied on self-report, whereas only a few studies applied observational methods in combination with questionnaires (Weigl et al., 2014; Weigl et al., 2013). Measures of care quality varied substantially across studies: Provider evaluations based on self-report, treatment outcomes were operationalized as adverse events (infections), while attainment of treatment goals (glycemic control), errors and malpractice claims were based on expert ratings, registry data, chart reviews, or insurance data.
Further caution stems from the potential omission of unpublished studies with negative or nil findings. Furthermore, potential confounding influences that strongly influence quality of care were not addressed as well as potential mechanisms that explain the observed associations.
Another important limitation refers to our confinement of physicians’ psychosocial work conditions. Some studies featured physicians’ work stress as the individual reaction to adverse psychosocial work conditions. This can also be considered as strain and raises concern over the specific causes of stress, that is, its attribution to the work environment or to physicians’ individual characteristics. Therefore we aimed to restrict our search to psychosocial work conditions as an external feature of the hospital work environment. However, we acknowledge that some studies analyzed work stress and that we excluded personal factors, that is, expertise and experience with stressful situations.
In this review, we did not address other specific work conditions of physicians that certainly can pose stressors. Specifically, we did not include working time regulations and work load for two reasons. Firstly, the literature base on work time directives, regulations and duty hour standards as well as work load and their substantial ramifications on quality of care are vast. Thus, these topics deserve reviews of their own, which is well acknowledged elsewhere (e.g., Goitein, Shanafelt, Wipf, Slatore, & Back, 2005; Landrigan et al., 2008; Morrow, Burford, Carter, & Illing, 2012) and has been conducted previously (Hickam et al., 2003; Kapinos et al., 2012). Secondly, we assume that the impact of extended working hours and work overload may be different from the above described pathways in which psychosocial work conditions lead to inferior quality of care, for example through fatigue and tiredness (Hickam et al., 2003).
Implications for clinical practice and future research
Our findings suggest various implications and call for further research to address the interplay of physicians’ work conditions and respective care outcomes.
First, quality of care is certainly influenced by many other systemic and organizational factors beyond physicians’ immediate work conditions, that is, training and skills of the individual as well as legislation and regulations in health care (Hoff et al., 2004). Thus, further research on physicians’ work life needs to address the broad scope of individual, work-related, organizational, and systemic determinants that contribute to high quality and safe care.
Secondly, our review was restricted to physicians. However, this professional group does not solely contribute to patient care. Nurses perform substantial functions with immediate patient contact. Future research may address potential differences in nurses and physicians in the relationship between adverse work conditions and care quality.
Thirdly, psychosocial work conditions are mainly responsible for the well-being and health of physicians. The work stress models cited in our review have been shown to explain substantial variance in the incidence of depression and myocardial infarctions, in and outside of healthcare professions (Angerer, Gündel, & Siegrist, 2014; Klein et al., 2011; Stansfeld & Candy, 2006). Moreover, the joint application of several work stress models increases the risk for poor health (Kivimäki, Vahtera, Elovainio, Virtanen, & Siegrist, 2007). Future approaches should disentangle the single as well as shared effects of established work stress models on physician well-being as well as care quality.
Fourthly, well conducted interventions on physicians’ work conditions and care quality are published (see Table 1-3 in the appendix). Inferior quality of care is an immediate threat to the economic success of any health care organization. Thus, improving the work life of health care professionals in general shall create a win-win situation towards a beneficial change in hospitals—in favor of physicians as well as their patients. A large Canadian intervention demonstrated that a participatory intervention has the potential to effectively improve work conditions in the hospital and health of employees (Bourbonnais, Brisson, & Vezina, 2011). Thus, drawing on established models of psychosocial work stress establishes an opportunity to conduct interventions on physicians’ work life as well as potentially promoting patient care.
Fifthly, the specific underlying pathways and mechanisms for the observed relationship between work conditions and quality of care were not examined in the reviewed studies. However, some publications provide discussion on this question. As suggested in our model, we assume that there are various work conditions in the hospital that interact with physician’s individual characteristics. This interplay eventually determines quality of care. We thus assume that different pathways exist, which translate adverse work conditions into suboptimal care. Intense knowledge about the root causes of unsafe or insufficient care helps to identify the determinants that contribute to the variance in health care quality, to define the impact of different clinical settings, to analyze the interplay of work conditions and quality, and to identify patient groups which are most sensitive to the sequelae of adverse working conditions of their physicians.
Finally, our findings shed light on specific work conditions of physicians’ work environment that can be subject to change and intervention. Perceived procedural justice, high alignment with the hospital management, a balance between effort and reward have been shown to positively affect health, motivation, and team work, which are all essential factors for good quality of care. An imbalance between efforts spent and rewards received in return result in poor commitment through low work motivation as well as low procedural justice (Siegrist, 1996; Virtanen et al., 2009; Virtanen et al., 2012). Both are essential for high-quality care, which is characterized by high levels of coordination and interdisciplinary team work. Moreover, justice has been positively associated with positive work attitudes and willingness to support decisions and decision-makers (Greenberg & Colquitt, 2005).
Conclusions
This review reported a comprehensive literature search on associations between physicians’ psychosocial work conditions and three major domains of quality of care. Our findings provide partial confirmation of our assumption that physicians’ psychosocial work conditions are directly related to quality of care. This review included several studies that applied different designs and measures in different clinical settings. Four intervention studies suggest that improvements in physicians’ work life positively influence quality of care by reducing errors and making patients more content with care. Preliminary evidence warrants extended and in-depth studies as well as interventions on physicians’ work conditions and quality of care outcomes.
References
- Alarcon, G. M., & Lyons, J. B. (2011). The Relationship of Engagement and Job Satisfaction in Working Samples. Journal of Psychology, 145(5), 463-480. https://doi.org/10.1080/00223980.2011.584083
- Angerer, P., Gündel, H., & Siegrist, K. (2014). Stress: Psychosocial work load and risks for cardiovascular disease and depression. Deutsche medizinische Wochenschrift, 139(24), 1315-1319.
- Bourbonnais, R., Brisson, C., & Vezina, M. (2011). Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occupational and Environmental Medicine, 68(7), 479-486. https://doi.org/10.1136/oem.2010.055202
- Buddeberg-Fischer, B., Klaghofer, R., Stamm, M., Siegrist, J., & Buddeberg, C. (2008). Work stress and reduced health in young physicians: prospective evidence from Swiss residents. International Archives of Occupational and Environmental Health, 82(1), 31-38. https://doi.org/10.1007/s00420-008-0303-7
- Carayon, P., Hundt, A. S., Karsh, B. T., Gurses, A. P., Alvarado, C. J., Smith, M., & Brennan, P. F. (2006). Work system design for patient safety: the SEIPS model. Quality and Safety in Health Care, 15, i50-i58. https://doi.org/10.1136/qshc.2005.015842
- Dekker, S. (2011). Patient safety: a human factors approach. : CRC Press. https://doi.org/10.1201/b10942
- Elovainio, M., Heponiemi, T., Sinervo, T., & Magnavita, N. (2010). Organizational justice and health; review of evidence. Giornale italiano di medicina del lavoro ed ergonomia, 32, B5-9.
- Fahrenkopf, A. M., Sectish, T. C., Barger, L. K., Sharek, P. J., Lewin, D., Chiang, V. W., & Landrigan, C. P. (2008). Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ 336 [7642], 488-491. https://doi.org/10.1136/bmj.39469.763218.BE
- Firth-Cozens, J. (2003). Doctors, their wellbeing, and their stress. BMJ, 326(7391), 670-671. https://doi.org/10.1136/bmj.326.7391.670
- Goitein, L., Shanafelt, T. D., Wipf, J. E., Slatore, C. G., & Back, A. L. (2005). The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Archives of Internal Medicine, 165(22), 2601-2606. https://doi.org/10.1001/archinte.165.22.2601
- Greenberg, J. (1990). Organizational justice: Yesterday, today, and tomorrow. Journal of management, 16(2), 399-432. https://doi.org/10.1177/014920639001600208
- Greenberg, J., & Colquitt, J. A. (2005). Handbook of organizational justice. : Psychology Press.
- Hickam, D. H., Severance, S., Feldstein, A., Ray, L., Gorman, P., Schuldheis, S., & …Helfand, M. (2003). The effect of health care working conditions on patient safety. Evidence Report/Technology Assessment (Summ) [74], 1-3.
- Hoff, T., Jameson, L., Hannan, E., & Flink, E. (2004). A review of the literature examining linkages between organizational factors, medical errors, and patient safety. Medical Care Research and Review, 61(1), 3-37. https://doi.org/10.1177/1077558703257171
- Johnson, J. V., & Hall, E. M. (1988). Job strain, work place social support, and cardiovascular disease: A cross-sectional study of a random sample of the Swedish working population. American Journal of Public Health, 78(10), 1336-1342. https://doi.org/10.2105/AJPH.78.10.1336
- Jones, J. W., Barge, B. N., Steffy, B. D., Fay, L. M., Kunz, L. K., & Wuebker, L. J. (1988). Stress and medical malpractice: organizational risk assessment and intervention. Journal of Applied Psychology, 73(4), 727-735. https://doi.org/10.1037/0021-9010.73.4.727
- Kapinos, K. A., Fitzgerald, P., Greer, N., Rutks, I., & Wilt, T. J. (2012). The Effect of Working Conditions on Patient Care: A Systematic Review In D. o. V. Affairs (Ed.),. Evidence-Based Synthesis Program.
- Karasek, R. (1979). Administrative Science Quarterly, 24. , 285-308.: , 285-308. https://doi.org/10.2307/2392498
- Kivimäki, M., Vahtera, J., Elovainio, M., Virtanen, M., & Siegrist, J. (2007). Effort-reward imbalance, procedural injustice and relational injustice as psychosocial predictors of health: complementary or redundant models? Occupational and Environmental Medicine, 64(10), 659-665. https://doi.org/10.1136/oem.2006.031310
- Klein, J., Grosse, K., Blum, K., & von dem Knesebeck, O. (2011). Psychosocial stress at work and perceived quality of care among clinicians in surgery. BMC Health Services Research, 11. https://doi.org/10.1186/1472-6963-11-109
- Koponen, A., Vahtera, J., Pitkäniemi, J., Virtanen, M., Pentti, J., Simonsen-Rehn, N., & Suominen, S. (2013). Job strain and supervisor support in primary care health centres and glycaemic control among patients with type 2 diabetes: a cross-sectional study. BMJ open, 3(5). https://doi.org/10.1136/bmjopen-2012-002297
- Landrigan, C. P., Fahrenkopf, A. M., Lewin, D., Sharek, P. J., Barger, L. K., Eisner, M., & Sectish, T. C. (2008). Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics, 122(2), 250-258. https://doi.org/10.1542/peds.2007-2306
- Lawton, R., McEachan, R. R., Giles, S. J., Sirriyeh, R., Watt, I. S., & Wright, J. (2012). Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Quality & Safety, 21(5), 369-380. https://doi.org/10.1136/bmjqs-2011-000443
- Lee, R. T., Seo, B., Hladkyj, S., Lovell, B. L., & Schwartzmann, L. (2013). Human Resources for Health, 11. , 48.: , 48. https://doi.org/10.1186/1478-4491-11-48
- Linzer, M., Manwell, L. B., Williams, E. S., Bobula, J. A., Brown, R. L., Varkey, A. B., & Schwartz, M. D. (2009). Working conditions in primary care: physician reactions and care quality. Annals of internal medicine, 151(1), 28-36. https://doi.org/10.7326/0003-4819-151-1-200907070-00006
- Mache, S., Vitzthum, K., Klapp, B. F., & Groneberg, D. A. (2012). Improving quality of medical treatment and care: are surgeons' working conditions and job satisfaction associated to patient satisfaction? Langenbeck's Archives of Surgery, 397(6), 973-982. https://doi.org/10.1007/s00423-012-0963-3
- McKinstry, B., Walker, J., Porter, M., Fulton, C., Tait, A., Hanley, J., & Mercer, S. (2007). The impact of general practitioner morale on patient satisfaction with care: a cross-sectional study. BMC family practice, 8(1). https://doi.org/10.1186/1471-2296-8-57
- Morrow, G., Burford, B., Carter, M., & Illing, J. (2012). Report for the General Medical Council. Durham: Durham University, Centre for Medical Education Research.
- Ndjaboue, R., Brisson, C., & Vezina, M. (2012). Organisational justice and mental health: a systematic review of prospective studies. Occupational and Environmental Medicine, 69(10), 694-700. https://doi.org/10.1136/oemed-2011-100595
- Nielsen, K. J., Pedersen, A. H., Rasmussen, K., Pape, L., & Mikkelsen, K. L. (2013). Work-related stressors and occurrence of adverse events in an ED. The American Journal of Emergency Medicine, 31(3), 504-508. https://doi.org/10.1016/j.ajem.2012.10.002
- Ross, S., Ryan, C., Duncan, E. M., Francis, J. J., Johnston, M., Ker, J. S., & Bond, C. (2013). Perceived causes of prescribing errors by junior doctors in hospital inpatients: a study from the PROTECT programme. BMJ quality & safety, 22(2), 97-102. https://doi.org/10.1136/bmjqs-2012-001175
- Rousseau, V., & Aube, C. (2010). Social Support at Work and Affective Commitment to the Organization: The Moderating Effect of Job Resource Adequacy and Ambient Conditions. Journal of Social Psychology, 150(4), 321-340. https://doi.org/10.1080/00224540903365380
- Shanafelt, T. D., Bradley, K. A., Wipf, J. E., & Back, A. L. (2002). Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine, 136(5), 358-367. https://doi.org/10.7326/0003-4819-136-5-200203050-00008
- Siegrist, J. (1996). Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology, 1(1), 27-41. https://doi.org/10.1037/1076-8998.1.1.27
- Stansfeld, S., & Candy, B. (2006). Psychosocial work environment and mental health - a meta-analytic review. Scandinavian Journal of Work, Environment & Health, 32(6), 443-462. https://doi.org/10.5271/sjweh.1050
- Tyssen, R., & Vaglum, P. (2002). Mental health problems among young doctors: an updated review of prospective studies. Harvard Review of Psychiatry, 10(3), 154-165. https://doi.org/10.1080/10673220216218
- Vincent, C., Moorthy, K., Sarker, S. K., Chang, A., & Darzi, A. W. (2004). Systems approaches to surgical quality and safety: from concept to measurement. Annals of Surgery, 239(4), 475-482. https://doi.org/10.1097/01.sla.0000118753.22830.41
- Virtanen, M., Kurvinen, T., Terho, K., Oksanen, T., Peltonen, R., Vahtera, J., & Kivimäki, M. (2009). Work hours, work stress, and collaboration among ward staff in relation to risk of hospital-associated infection among patients. Medical care, 47(3), 310-318. https://doi.org/10.1097/MLR.0b013e3181893c64
- Virtanen, M., Oksanen, T., Kawachi, I., Subramanian, S. V., Elovainio, M., Suominen, S., & Vahtera, J. (2012). Organizational justice in primary-care health centers and glycemic control in patients with type 2 diabetes. Medical care, 50(10), 831-835. https://doi.org/10.1097/MLR.0b013e31825dd741
- Weigl, M., Hoffmann, F., Muller, A., Barth, N., & Angerer, P. (2014). Hospital paediatricians' workflow interruptions, performance, and care quality: a unit-based controlled intervention. European Journal of Pediatrics, 173(5), 637-645. https://doi.org/10.1007/s00431-013-2232-z
- Weigl, M., Hornung, S., Angerer, P., Siegrist, J., & Glaser, J. (2013). BMC Health Services Research, 13. , 401.: , 401. https://doi.org/10.1186/1472-6963-13-401
- Weigl, M., Hornung, S., Petru, R., Glaser, J., & Angerer, P. (2012). Depressive symptoms in junior doctors: a follow-up study on work-related determinants. International Archives of Occupational and Environmental Health, 85(5), 559-570. https://doi.org/10.1007/s00420-011-0706-8
- Weigl, M., Müller, A., Vincent, C., Angerer, P., & Sevdalis, N. (2012). The association of workflow interruptions and hospital doctors' workload: a prospective observational study. BMJ Quality and Safety, 21(5), 399-407. https://doi.org/10.1136/bmjqs-2011-000188
- West, C. P., Huschka, M. M., Novotny, P. J., Sloan, J. A., Kolars, J. C., Habermann, T. M., et al., et al. (2006). Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA 296 [9], 1071-1078. https://doi.org/10.1001/jama.296.9.1071
Appendix
Table 1
Physicians’ psychosocial work conditions and physicians' and/or patients' perception of the quality of care.
Table 2
Physicians psychosocial work conditions and success of treatment or absence of complications.
|
Citation (first author, year) |
Design of study (observational/interventional) and primary research question |
Physicians studied |
Patients studied |
Measurement of work conditions |
Measurement of quality of care |
Main results (extracted) |
|---|---|---|---|---|---|---|
|
Observational, cross-sectional study Objective: Associations between healthcare personnel’s perceived job strain, supervisor support and the outcome of care in terms of glycemic control among patients with type 2 diabetes. |
Physicians (n=122) and nurses (n=300) in 18 primary care health centers (response rate 78%) |
Type 2 diabetes mellitus (n=8975) (from register data of all patients treated in these health centers) |
Job strain, supervisor support Covariates included in analysis: patient sex and age, organization characteristics (the percentage of temporary employees and the mean rate of sickness absence days in the HC), HC service area characteristics (educational level of the residents, median income and unemployment rate). |
Achievement of good blood glucose control (HBA1c < 7 mg/dl) |
||
|
Observational, cross-sectional study Objective: Association between perceived organizational justice among health care providers and glycemic control among their diabetic patients. |
Physicians (n=122) and nurses (n=300) in 18 primary care health centers (response rate 78%) |
Patients with Type 2 diabetes mellitus (n=8954) (from register data of all patients treated in these health centers) |
Staff-reported procedural justice and relational justice, effort-reward imbalance, and work-unit team climate Covariates included in analysis: patient-level and unit-level (for details see Koponen et al., 2013) |
Achievement of good blood glucose control (HBA1c < 7 mg/dl) |
|
|
|
Observational, cross-sectional study Objective: Association between work hours, work stress, and collaboration among the ward personnel, and the risk of hospital-associated infection among patients. |
Physicians (n=73) and nurses (n=999), other (=87), from 60 (non-psychiatric) wards in 6 hospitals Overall response rate in the survey 77% |
All patients (n = 1092 from 1102) included, on one sampling day for each ward (32% on surgical wards, 34% on internal wards) |
Working hours per day were calculated from staff responses (used as a dichotomous variable of 8.75 hours; i.e., 8 hours 45 minutes per day vs. less). Work stress was assessed with scales of the job strain model, and the effort-reward imbalance (ERI) model. Covariates included in analysis: patient sex, age, surgical status, exposure to devices, hospital type, unit type, number of patients at ward, diagnosis of cancer (lymphoma, leukemia, or myeloma), and use of corticosteroids. |
Prevalence surveillance was performed by 4 infection control nurses, using standard criteria to register hospital-associated infection. |
|
|
|
Observational, cross-sectional study Objective: To assess the relationship among adverse primary care work conditions, adverse physician reactions (stress, burnout, and intent to leave), and patient care. |
Family physicians and general internists (n=449) from 119 practices (59.6% of those invited) consented to participate, and 422 (94.0%) completed the baseline survey (participation rate, 56.0%). |
1795 patients, an average of 4 per physician (range, 1 to 8 patients) with diabetes, hypertension, or heart failure. |
Survey among physicians (items chosen based on focus groups). physician perception of clinic workflow (time pressure and pace), work control, and organizational culture (assessed survey); physician satisfaction, stress, burnout, and intent to leave practice (assessed by survey); Covariates included in analysis: physician age, sex, race, and clustering within clinics |
Health care quality and errors (assessed by chart audits). |
|
Table 3
Physicians’ psychosocial work conditions and prevalence of medical errors.